Menopause: Everything You Need to Know
We've got the doctor-approved details on menopause causes, symptoms, treatments, and a jillion other facts and tips that can make life with menopause easier—and less sweaty.






Menopause is a phase of life that affects a full half of the population—yet in many circles, it remains “taboo,” with women embarrassed to discuss it. Just as #noperiodshame has begun sparking open conversation about a completely normal biological process, it’s time for menopause stigma—internal and external—to end, too. Whether you’re wondering about early signs, experiencing hormonal shifts, or are already in full menopause and looking for the best treatments so you can feel like yourself again, we at HealthCentral are here to help.
What Is Menopause, Actually?
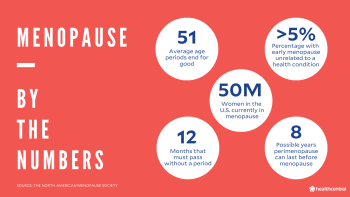
Though it's got the word “pause” in it, this life stage would more aptly be called menostop (you heard it here first!). That's because the official definition of menopause is when you haven’t had a period in over a year (or, in other words, for 12 consecutive months). It’s triggered by age-related hormonal shifts, though these can actually start (eep) a decade before you hit true menopause. More than 60 million women in the United States are currently in menopause, so while it may seem like nobody's talking about it, you are certainly not dealing with this transition alone.
What Causes Menopause?
Every woman is born with a finite number of eggs. As we age, the ovaries begin to slow in releasing functioning eggs—until they stop when we have no functioning eggs left. At the same time, the ovaries begin to produce less and less of the reproductive hormones progesterone and estrogen——the first triggers the lining of the womb to grow so it can house a fertilized egg, while the second helps with that but also keeps the growth of that lining in check so it doesn't get too thick, leaving adequate room for the egg to grow. (When the egg isn't fertilized, the lining sheds, and you get your period.)
Here’s a simple step-by-step:
The eggs in your ovaries are surrounded by cells that make up what’s known as the follicle.
As the egg matures, the follicle cells multiply, and the follicle begins to secrete estrogen.
Once the egg is released from the ovary, the empty follicle, left behind, then also begins to put out progesterone and estrogen—the hormones that help your body prepare for that just-released egg to be fertilized and settle in for the long haul.
But remember, you have a set number of eggs—so eventually, the number of functional eggs decline and you eventually just run out. When there are no more eggs or follicles, your ovaries stop—or at least drastically reduce—their production of the two reproductive hormones
At that point, your periods usually become less frequent and often lighter, though for some women they do the opposite and become heavier, longer, and closer together; both types of period changes are normal before menopause. When you no longer menstruate at all—because there are no eggs to release—the process is complete: You’re in menopause.
When Will I Go Through Menopause?
There is a wide range of ages at which women hit menopause, though on average, the magic year is 51.
That doesn’t mean symptoms wait till then, however. You may be in pre-menopause, also called perimenopause, as early as your mid-30s to late 40s. The typical length you’d be in perimenopause is four years, but it can last as long as 10 years (!) or be as short as a few months. To be clear, perimenopause is not the actual beginning of menopause; it’s the period of time that occurs before the big M.
During perimenopause, shifts in hormones may cause a wide array of symptoms. Period changes—whether they are further apart or closer together, longer or shorter, heavier or lighter—are the first indicator that you have entered Perimenopause Land (welcome!). Other physical and psychological changes can include trouble sleeping, mood swings, weight gain, or a lack of interest in sex. Sometimes, especially if you experience these symptoms on the earlier side—say, in your 30s—you might mistake them for a reaction to stress or simply to the bombardment of a busy life, as opposed to the result of hormonal shifts.
There are also two conditions known as early menopause, menopause before age 45, and premature menopause, which occurs before 40. These are uncommon phenomena without contributing factors. In fact, fewer than 5% of women go through early or premature menopause without having other health conditions.
Most often, early or premature menopause happens because a woman has had a hysterectomy with removal of the ovaries, whether because of ovarian or cervical cancer, fibroids, or some other reason. Chemotherapy (with or without surgery) can also damage your ovaries and trigger early menopause. One other potential predictor of early menopause: if one or more of your female relatives experienced it.
Do I Have the Symptoms of Perimenopause or Menopause?
Any of the below symptoms can signal that you’re starting perimenopause, and they usually accelerate as you get closer to actual menopause; once you hit menopause, these symptoms can continue for months or even years afterward (the average: four to five years).
You probably won’t have all these symptoms, but every woman's experience is unique. Intermittent symptoms, like hot flashes, might go away as your body adjusts to the lack of estrogen in your body—in fact, some women who take hormone therapy (more on that in a minute) find that when they stop, that’s when they get hot flashes. Other symptoms, like vaginal dryness, might just become a fact of post-menopausal life.
Among the most common symptoms of perimenopause and menopause:
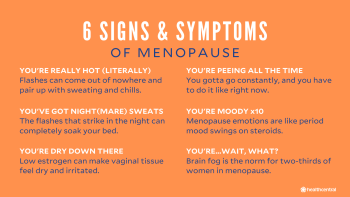
Hot Flashes. Feeling suddenly hot and bothered, but temperature-hot and actually bothered (a.k.a.: the sucky, not sexy, “hot and bothered.”) These can come on at any time, along with flushing, your heart speeding, sweating, and even chills. They can last 10 seconds or go on for three to five minutes. Some women get hot flashes daily, some just a few times a week—it’s incredibly variable.
Night Sweats. Hot flashes that happen at night—they can wake you in a pool of your own sweat.
Insomnia. Think of how you feel when too toasty in a room at night. Explains why that lovely p.m. perspiration can keep you awake. Worsening the issue? General aging creates an increased sensitivity to caffeine, more difficulty dozing off, and less deep sleep.
Urinary Frequency or Urgency. Feel like you have to pee more frequently? Blame the decrease in estrogen levels. It’s also responsible for making it difficult for you to hold it when you really do have to go—further compounding sleep issues, all while feeling the bathroom urge at night.
Mood Swings. If you experienced anger or sadness during PMS while you were menstruating, or had postpartum depression earlier in life, you are more likely to have the same symptoms from menopausal hormone dips, though they can also affect women with no prior history. This can include crying jags or feeling quicker to anger than usual.
Depression and Anxiety. Similarly, if you had bouts of depression or anxiety before menopause, you are more likely to see them reappear. This can happen for both physical reasons (changing hormone levels can disrupt the smooth working of your brain’s neurotransmitters and throw your moods off track) and psychological ones—it can be disorienting to go through any life change, especially one that means you’re coming to the end of your fertile years. Plus: Insomnia! Hot flashes! It’s normal if those are upsetting.
Vaginal Dryness and Pain During Sex. Dipping estrogen. Again. It can make vaginal tissue feel dry and irritated, resulting in less natural lubrication, which can lead to painful microabrasions from the friction of sex. This is technically called genitourinary syndrome, which can also lead to an increased risk of infections including urinary tract infections and bacterial vaginosis.
Loss of Libido. That hormonal drop + the resulting vaginal dryness and irritation can make some women feel less interested in sex altogether.
Memory Changes and Brain Fog. About two-thirds of women going through perimenopause and menopause have a harder time remembering things and focusing. Additionally, a recent study published in the journal Climacteric showed that while most women do not experience severe cognitive impairment during menopause, a significant minority experience weaknesses in verbal learning and memory.
How Long Does Menopause Last?
Symptoms are usually most pronounced in the first two years of menopause, and for some women, the issues tend to subside after they’ve been in menopause for a year or two. Unfortunately, though, it’s not uncommon for these side effects to stick around for as long as eight to 10 years, beginning in perimenopause and continuing for four to five years after menopause.
What Is the Best Treatment for Menopause?
The first thing to know is that you don’t have to treat menopause at all. This isn’t an illness, it’s a natural process. But there are lots of things you can do to help lessen (and, for some women, eliminate) the symptoms.
For hot flashes and night sweats:
The most effective treatment to stop them is hormone therapy (or HT). (This is also known as menopausal hormone therapy, MHT, and was previously called hormone replacement therapy, or HRT). Your doctor will prescribe a very low dose of estrogen, sometimes combined with progesterone. Most hormone replacements are pills, but there are also skin patches, vaginal creams and gels, and vaginal rings.
There’s been controversy about the safety of hormone therapy. Based on the latest research, FDA-approved hormone therapies are safe for the majority of women having menopausal symptoms when taken under a doctor’s supervision and for a finite period of time.
That doesn’t mean there aren’t risks, though. Women who have or have had breast, ovarian, or endometrial cancer shouldn’t take hormone therapy. Neither should women who have had stroke. For some women, hormone therapy may increase their chance of heart attack, stroke, and breast cancer; you and your doctor will need to carefully go over your risk factors and decide whether this is the right treatment for you.
Now, this is different for women who go through premature or early menopause. They are at higher risk of cardiovascular disease (as well as bone loss and insulin resistance), and FDA-approved hormone therapy is recommended. In this age group (as opposed to women in their 50s or 60s), HRT helps prevent heart risks while also alleviating other common symptoms of menopause.
No matter what your age when you start HT, most docs will want to re-evaluate every three to six months. For one thing, you might have better results with different dosages and timing—you and your doctor might decide to try several different protocols. For another, if the hormone therapy isn’t giving you relief from your symptoms (everybody’s experience varies), you might want to stop it altogether.
For vaginal dryness and pain during sex:
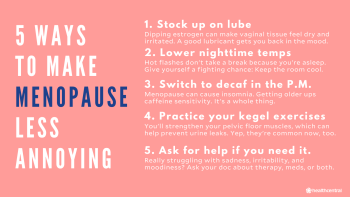
HT is also a first-line treatment for dryness and the irritation it can result in—in this case, your doctor will prescribe the therapy in the form of a vaginal ring, pill, suppository or cream rather than orally. HT helps some women regain their sex drive, but if that’s not your problem, or you just want to try a nonprescription treatment, you can also use an over-the-counter vaginal moisturizer or lubricant (K-Y, Replens, Astroglide—there are lots of versions at the drugstore).
There’s some evidence that cannabis—both THC (the compound that makes you “high”) and CBD, the cannabis plant’s other main component—can increase sex drive. However, there are studies that have found just the opposite. If your loss of libido is related to anxiety—maybe you’re less prone to have sex because you worry about your lack of lubrication or just feel uncomfortable with the changes your body is going through—then it might be worth trying cannabis sheerly for its ability to lower inhibitions. This is a total personal-choice call, but definitely don’t underestimate the boons to your overall health that regular (non-painful!) sex can have.
For depression and mood changes:
Just as with depression at any stage of life, it’s worth considering taking antidepressants to help with the sadness, irritability, and moodiness that often accompany menopause. Treating those symptoms can also make way for a return in libido, and some women find that a low dose of antidepressants can lessen hot flashes (finally, a bonus). As with any prescription, your doctor can help choose the right medication and work with you to fine-tune how much of it you take, how often, and for how long. (Some antidepressants can dull libido, for instance, so you'll want to make sure your M.D. knows if that's already an issue for you.) It’s also worth talking to a therapist about how you’re feeling—or even just to others going through menopause.
For insomnia:
Though there are certainly medications you can take for insomnia (both prescription and over-the-counter), your doctor is likely to recommend that you look at lifestyle factors first: Are you drinking too much caffeine? Using your smart phone or tablet right before bedtime? Keeping your bedroom too warm? Avoiding all of these things can help you fall asleep faster, snooze more restfully, and cut down on middle-of-the-night wakeups.
For the urge to urinate:
Here, too, behavioral changes might help:
Cut back on the coffee and soda (yep, and on alcohol, too)
Do Kegel exercises (contract and relax the muscles in your pelvic and genital area) regularly to strengthen your pelvic muscles, the ones that control urine flow.
Try taking an exercise class that focuses on strengthening the entire pelvic floor, such as Pilates, which can also have the added benefit of improving sex.
Are Natural Menopause Remedies Effective and Safe?
There’s been a lot of buzz around bioidentical hormones, which are molecularly identical to the hormones women’s bodies naturally make but are constructed with plant chemicals (mostly from yams and soybeans); manufacturers often market them as “natural.” There are FDA-approved options (including bioidentical and naturally derived choices) that are safe because they have been tested and have set amounts. But don’t be tempted by non-FDA approved hormones, which you can get without a prescription. They can vary in strength and concentration by a dangerous degree.
You’ve surely noticed the slew of natural menopause supplements at your local drugstore, too. Some herbs and supplements, such as maca and black cohosh, have been found in studies to be effective at controlling menopause systems, especially hot flashes. There have also been studies showing that these non-prescription remedies don’t do any better than a placebo—so while they’re not dangerous, you could take a sugar pill and get the same result.
But hey, that placebo effect is still an effect, so if you want it, we don’t blame you! Just don’t DIY this. There’s a huge array of supplements out there, and that’s before you even think about the range of doses you might take or the combinations of remedies. Always talk to your doctor before trying anything new. If you’re already on hormone therapy, you need to be especially vigilant about discussing over-the counter remedies with your doctor—there could be adverse reactions, or you might be undermining the work the HT is doing.
Where Can I Find Menopause Communities?
If you’re going through menopause, you really are in good company: Remember, a gajillion other women in this country are menopausal, too. If you need more information or just want somebody to talk to who gets it immediately, check out these resources.
Top Menopause Instagrammers and Blogger
Anna Cabeca, D.O., @drannacabeca, https://drannacabeca.com
Follow because: Dr. Cabeca doesn’t just know what it’s like to go through menopause, she’s also triple-board certified (in internal medicine, obstetrics and gynecology, and regenerative and anti-aging medicine), so she fully understands the science behind menopause. She recommends integrative approaches to make sure you thrive, not just survive, the transition.
Meg Matthews, @megsmenopause
Follow because: It’s not just her menopause, it’s yours, too. She poses questions to foster conversation, so each post is like its own open forum. It doesn’t hurt that she does it with such style, either: The uber-fashionable Matthews is a columnist for Red magazine and was a former music-industry events planner and designer for the Brit Pop scene in the '90s.
Jo Harvey-Graham, @50sowhatofficial
Follow because: She’s 50, and so what — who said life couldn’t be fabulous at 50 and beyond? So she pairs up with docs to do Q&As about hormones and menopause in her stories, and she posts other fabulous fifty-year-olds on her feed, while keeping things light, cool, and real. Like, can’t hold your bladder, sprouting warts, so. many. greys, and more – kind of real.
Top Menopause Podcasts
The Happy Menopause. Yes, according to registered nutritional therapist Jackie Lynch, you can be happy during menopause. She focuses on mind-body and nutritional approaches to managing mid-life hormonal changes.
The Flipping 50 Show. While the main focus of this podcast is on menopause,it also touches on everything else that changes when you’re approaching or past 50, including how your fitness, diet, and lifestyle should all shift with your age—and not in a “your life is now over” kind of way. The tips are trustworthy: Host Debra Atkinson is a fitness pro (she’s a certified trainer with a master’s in exercise and sports psychology) and wellness coach.
Top Menopause Support Groups and Non-Profits
The North American Menopause Society (NAMS). This nonprofit has a function where you can enter your zip code and find doctors in your area who have gone through the NAMS Certified Menopause Practitioner (NCMP) program. Meaning: a doc who really gets it.
Red Hot Mamas. Created by Karen Giblin—who in 1991, when she held public office in Connecticut, had a total abdominal hysterectomy and bilateral oophorectomy—this group’s goal is to outsmart menopause. How? With tons of evidence-based guidance paired with insights from the menopause community. These are your type of people: smart, sassy, and supportive.
American Society for Reproductive Medicine. For when you want the details in legit medical terms so that when you’re talking to your doctor (and you should), you’re speaking their language.
51, but it varies from woman to woman. Pre-menopause—a period of time when symptoms begin but during which you still have your period—can begin in your mid-30s. Only a small percentage of women go through early menopause, which is considered before age 40.
When you’re in true menopause—your periods have stopped with no interruptions for a full 12 months—you are no longer fertile and cannot get pregnant. But don’t throw caution (or a condom) to the wind if you’re in perimenopause (you have menopausal symptoms but still get a period, even if only sporadically): At this point, your reproductive hormones and functional eggs are declining, but it is still possible to get pregnant.
As we age, our metabolism slows down, and we begin to lose muscle mass, so we need to consume fewer calories (but often don’t). The lower estrogen levels that are a part of menopause also cause our metabolism to get sluggish, so it’s a double whammy. Add in menopause’s typical sleep issues, and you may exercise less and snack more. No matter what the cause, the fix is familiar: Eat fewer calories, avoid sugar and simply carbohydrates that quickly convert to sugar, and exercise as regularly as you can.
Not yet, but it looks you’re headed that way (barring some medical reason for a lack of periods). If you’re beginning to experience more time between your periods, lighter periods, or just a general “I’m not sure what in the heck is happening with my periods!”, you’re likely in perimenopause—think of it as the lead-up to menopause. It can last a few months or a few years. True menopause is defined as when your periods have stopped altogether for one year.



