Multiple Sclerosis: Everything You Need to Know
Get the doctor-approved details on causes, symptoms, treatments, and other facts and tips that can make life with MS easier.






Whether you’ve just been diagnosed or worry you could have multiple sclerosis (MS), you’re probably nervous, confused, and a little scared. That’s a natural reaction, and everyone featured on HealthCentral with a chronic illness felt like you do now. But we—and they—are here for you. On this page, you’ll discover the realities and challenges of the condition, but also the best treatments, helpful lifestyle changes, where to find your MS community, and all the crucial information to help you not merely manage—but thrive. We’re sure you’ve got a lot of questions ... and we’ve got the answers you need. Read on.
What Is MS, Anyway?
It’s easy to think that multiple sclerosis is caused by some kind of neurological disorder since it, you know, affects your brain, spinal cord, and optic nerves (a.k.a. the central nervous system, or CNS). But MS is actually an inflammatory autoimmune disease. As you may know, autoimmune diseases occur when the immune system mistakenly attacks healthy tissue in the body. In MS, the target is myelin, the fatty tissue that protects your nerve cells in the CNS.
Eventually, this damage (a process called demyelination) creates scars on your brain and spinal cord. And it's these lesions that disrupt the flow of information that usually zips through your nerves so you can do all the things you do. The presence of lesions on your brain is a lot like the fingerprints left behind at a crime scene—when doctors spot them, they know that MS is the likely suspect.
In fact, that’s why MS is called MS. “Sclerosis” means scarring. “Multiple” means more than one. So, multiple sclerosis = MS. To really understand how MS affects the cells, it helps to have a little context on how nerve cells work in the first place.
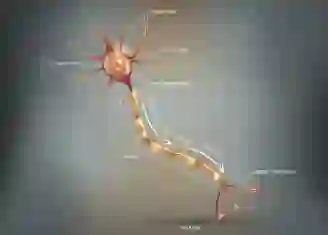
All nerve cells, also called neurons, have distinct parts. Here's what they do:
The dendrites on the cell surface receive (like an antenna) electrical messages (commands) from both the brain and sensory organs (such as your eyes and ears).
The soma is the cell body. It doesn’t play an active role in transmitting nerve impulses; the signals simply pass through it.
The axon is the nerve fiber that actually transmits these messages. Think of an axon like a wire carrying an electric current.
Axon terminals are the ends of the axon fibers.
Synapses transmit the message onto the next nerve.
The axons are what you’ll be interested here, because damaged axons are what reeeally cause the confusion, dysfunction, and/or pain that come with MS. We’ll spare you the nitty gritty, but here’s what you need to know:
When the axons send their messages through the CNS, they rely on the myelin sheath for insulation. Myelin coats the nerves and essentially keeps these signals running smoothly.
When myelin is stripped, the signals go a little haywire. This occurs after a breakdown of the blood-brain barrier, which we all have to protect our brains from invading pathogens. While researchers still aren’t certain why this breakdown occurs in people with MS, they do know a broken or leaky blood-brain barrier allows certain immune cells to cross over into the brain, which then cause inflammation. And inflammation not only makes the barrier even leakier, it also disrupts communication between the nerves by stripping the myelin sheath, eventually leading to scarring—or sclerosis—on your brain.
Bottom line? All these changes to the nerves can bring a whole constellation of symptoms, including eye pain and vision problems, motor challenges, changes to the bladder and bowels (having to pee urgently far too frequently, for example), plus trouble focusing and remembering. And they’re different for everyone. Your experience with MS may vary greatly from the person sitting across from you in the waiting room.
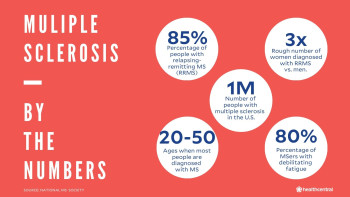
About a million people in the U.S. have MS, and about 2.8 million people have it worldwide. MS is three times more common in women than in men, suggesting that sex hormones such as estrogen and testosterone may play a role in the development of the disease, although researchers are still looking into this theory. There isn’t a cure—yet—but there are loads of treatment options. And while MS is a progressive disease, doctors and patients have plenty to be hopeful about.
A generation ago, medicinal treatment for MS symptoms did not exist. People with MS now enjoy a quality of life unknown even a decade or two ago. Science may not—yet—have all the answers, but it’s asking the right questions. Your job is to live as healthfully—and happily—as possible until all the answers arrive. And like we said from the start—we’ve got you.
The Types of Multiple Sclerosis
Here’s the thing about MS…it’s not just one thing! In fact, there are four possible diagnoses (and one condition that may be a precursor):
Clinically Isolated Syndrome: CIS can be an early indicator of MS. It refers to the first symptoms of MS that last at least 24 hours. But not everyone diagnosed with CIS goes on to develop MS, and not everyone diagnosed with MS is diagnosed at this earliest stage.
Relapsing-Remitting (RRMS): This is the most common form of MS. About 75% to 85% of people with MS are initially diagnosed with it. RRMS simply means that disease symptoms flare, or relapse, for periods of time—at least 24 hours, but up to weeks or even months—and then retreat, or remit, into remission. Remission periods, when symptoms go away completely, can last for years.
Secondary-Progressive (SPMS): SPMS refers to a stage of MS when symptoms steadily worsen, with or without periods of remission. Before disease-modifying therapies (DMTs) were first introduced in the mid-1990s, it was thought that 50% of all people with RRMS would go on to develop SPMS about 10 years after their initial diagnosis. While long-term data isn't yet available, many doctors believe today's treatments for RRMS will significantly delay its onset.
Primary-Progressive (PPMS): Only 10% of people with MS develop this manifestation of MS, which is known for steadily worsening symptoms from the outset of the disease, with no periods of relapses or remissions.
Progressive-Relapsing MS (PRMS): Affecting just 5% of people with MS, PRMS is the rarest form of the disease, known for its steadily worsening symptoms and acute (severe) relapses, with or without recovery.
What Are the Different Types of MS?
The disease is divided into four categories, but most people fall into the first one.
What Causes MS?
Like so many autoimmune diseases, we still don’t know what exactly triggers the onset of MS. We know the immune system goes into overdrive. We know the nerve cells get damaged. But the root cause? Still under investigation. As frustrating as that is, researchers do know a lot about what may increase your risk for the condition.
Some of the most important risk factors related to MS are:
Sex: Women are two to three times more likely than men to have RRMS (by far, the most common type). Research suggests there may be a link between sex hormones like estrogen and testosterone, which affect the immune system and the development of MS. Estrogen makes the immune system more reactive, perhaps an indicator of why women get more forms of MS with much higher frequency. That said, men are just as likely as women to develop PRMS, the most severe type of this disease.
Age: Although MS can occur at any age, there are some peaks: RRMS usually begins in the 20s and 30s. On average, SPMS is diagnosed about 10 years later than RRMS, but new advances in treatment mean that fewer people with RRMS are actually shifting into SPMS. Most people with primary-progessive MS are about a decade older than those who develop the relapsing-remitting form. And PRMS is generally detected in both men and women who are in their mid-to-late 30s.
Family History: People who have parents or siblings with MS are more likely to develop the condition. Although MS is not an inherited condition, it likely has a strong genetic susceptibility. According to the MS Trust, more than 230 genes have been found to increase the risk of developing this disease. None individually cause MS, and every person will have a different combination of these genes. But because family members share many of the same genes, your risk is higher if you have a family member with MS.
Mononucleosis as a Teen/Young Adult: While research hasn't yet made a direct connection between the Esptein-Barr virus (EBV), which causes most cases of mono, and MS, multiple studies have shown associations between the two, especially among those who experienced EBV infection as teenagers or young adults, when the illness tends to be more severe than in young children.
Smoking: Smoking is a known risk factor for MS, possibly in part because it causes inflammation throughout the body.
Geography: MS is far more common in countries with temperate or cool climates, including Canada, the northern U.S, parts of New Zealand and southeastern Australia, and Europe. Why? Research has found that the further away people live from the equator—likely because they are exposed to less sunshine—the more common MS is.
Vitamin D: Low levels of vitamin D have been linked to a greater risk of MS. Because vitamin D mostly comes from sunlight, a D deficiency may be the likely culprit for higher rates of the disease in more temperate, or cooler, climates.
What Are the Symptoms of MS?
Here’s the thing: MS is truly an individual condition. Its progression and symptoms present differently in everyone with the disease. That’s because MS affects different parts of the central nervous system differently in different people. (Say that three times fast.)
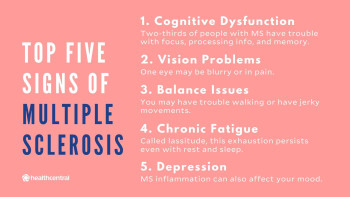
That’s not to say there aren’t common symptoms—there are. But which specific symptoms someone with MS gets, and in what order, will vary depending on where MS lesions form. And sometimes, the location of the lesion doesn’t exactly correspond to the symptom! It’s annoying like that. That said, here are some common threads:
Vision problems: Eye problems, known as optic neuritis, can be the first sign of MS that lead to the initial diagnosis of this disease, likely because they can’t be written off as easily as, say, fatigue (“Isn’t everybody tired?”) or memory issues (“We all forget things, right?”). When your vision is suddenly blurry or your eyeball starts to hurt, you don’t wait around. You see the doctor.
Cognitive problems: More than half of all people with MS will experience trouble with thinking, concentration, and memory, and if it’s happening to you, it’s likely very distressing. It may also be the reason you first sought help, or even received a diagnosis of this disease.
Fatigue: Feeling deeply exhausted is a hallmark symptom of MS, and this exhaustion is thought to be the primary reason for early departure from the workforce among people with MS. And we’re not talking your typical “I need a 20-minute nap” kind of tired here. We’re talking “It’s-tough-to-get-out-bed-all-day” fatigue, sometimes for days on end, and it’s present in about 80% of people with MS. Dealing with chronic inflammation requires boatloads of energy, and sometimes your body just can’t keep up.
Depression: Studies reveal how people with MS experience higher rates of clinical depression than the general population. However, people with MS who are depressed share similar rates to people with other chronic inflammatory conditions, such as rheumatoid arthritis (RA) and inflammatory bowel diseases such as ulcerative colitis and Crohn’s, which may suggest that inflammation helps fuel symptoms of depression.
Weakness: Your body might feel weak for any number of reasons if you have MS. For starters, impaired nerve conduction between the CNS and your body’s muscles may make those muscles work less efficiently, leaving you with a weakened feeling all over. And, of course, once you stop using those muscles with regularity, your endurance levels fall—so it can be a bit of a vicious cycle.
Numbness and tingling: Maybe you experience “pins and needles” in one leg or notice significantly less feeling in one hand (or bare foot) when it touches something than the other. People with MS have diminished, altered, or even total loss of sensation in different part of their bodies, which is sometimes accompanied by a tingling sensation.
Walking problems: Numbness is not the only thing that can negatively affect your ability to walk. Many people with MS have jerky movements and difficulty walking because the myelin on the nerves that control the arms and legs is damaged. Involuntary muscle spasms (called spasticity) are common in people with MS, too. Electric shock-like sensations called Lhermitte’s signs, which begin in the neck and radiate down in the trunk and the legs, can also make walking difficult.
Bladder and bowel problems: Do you feel like you need to pee urgently, and all the time? These symptoms can happen when MS lesions disrupt nerve signals from the brain to the bladder and bowels—and they can be devastating, because you might feel humiliated with a growing lack of control over how often, and where, you choose to relieve yourself.
Sexual issues: According to one study of people with MS, 63% reported having sex less frequently after being diagnosed with this disease. Other research shows that 91% of men and 72% of women with MS surveyed reported sexual problems. Men with MS may have difficulty achieving, or sustaining, an erection. Women with MS may have reduced clitoral sensation. These stats are alarming, we know, so be sure to share any symptoms with your doctor, who can help you navigate these changes to your sex life.
Additional MS Symptoms:
Slurred speech, which can result from cognition problems
MS hug, also known as girding or banding. This is an uncomfortable feeling of tightness around the torso that may cause difficulty breathing and can result from muscle spasms, nerve damage, or both.
Seizures caused by lesions on the brain. These are relatively rare—just 2% to 5% of people with MS experience them at varying intervals—and they're treatable with medication.
Difficulty breathing, which is less common and sometimes related to pre-existing allergies, illnesses like bronchitis or pneumonia, or sleep apnea.
Dizziness or vertigo, which is a spinning sensation and is quite common. It's usually treated with anti-motion medications.
Pain, which may feel like burning, stabbing, sharp, or squeezing sensations
Itching, which is part of the family of abnormal sensations associated MS nerve damage that includes “pins and needles” and the types of pain described above.
How Is MS Diagnosed?
Unfortunately, there is no single, defining test for multiple sclerosis. Rather, doctors will only conclude that you have MS after systematically ruling out other diseases—including Lyme disease, HIV, lupus, brain tumors, and spine conditions, to name a few—that might be causing your symptoms. When—and only when—all signs point to MS will you get what’s called a diagnosis of exclusion or differential diagnosis.
A healthcare team may begin to suspect MS from the outset based on who the patient is and what the symptoms are. For example, a woman in her 20s or 30s with vision problems and pain behind one eye—strong indicators of optic neuritis, which is often a first symptom of MS—is usually a candidate for multiple sclerosis.
However, because MS symptoms are so wide-ranging, diagnosing it can sometimes be difficult. A man in his 50s with symptoms centered around emotional or cognitive problems might initially get a diagnosis of a stroke, for example.
Doctors use many different tests and tools to narrow down the cause of symptoms. These can include:
Physical exam
Medical history, including a family health history
Magnetic resonance imaging (MRI), an imaging test that uses powerful magnets and computer waves to make a detailed picture of your brain and spinal cord, which may show signs of scarring
Spinal tap to examine cerebrospinal fluid that runs through the spinal column, which may show signs of the immune system attacking itself—if you have MS, this fluid will contain higher levels of a protein called immunoglobulin, which usually indicates inflammation in the brain
Evoked potentials, which are electrical tests to see if MS has affected the pathways of your nerves
Blood tests to rule out other possible conditions, such as Lyme’s disease
Of these methods, MRIs and spinal taps can sometimes produce the most solid clues. MS lesions are an important sign of MS and can show up directly on an MRI scan. If a person has lesions throughout the brain—called lesion burden—then an MS diagnosis is much easier to make. The same goes for the presence of high levels of immunoglobulin in your spinal fluid.
With so many step-by-step tests to be done, and with other conditions in need of being ruled out, a diagnosis can take anywhere from weeks to months.
What Are the Treatments for MS?
There is no cure for MS yet, although treatment has come a long way in the last two decades. The best approach is a comprehensive one where you, along with your team of doctors, work to manage and prevent disease flares using a combination of medications, preventative strategies, and healthy living choices.
Disease-Modifying Therapies (DMTs)
According to the National MS Society, more than two dozen disease-modifying medications (DMTs) have been approved by the U.S. Food and Drug Administration (FDA) to treat RRMS. Of this group, one—ocrelizumab, sold under the brand names Ocrevus—has been approved to treat both RRMS and PPMS, with a few others are approved for SPMS and CIS.
Some DMTs are biologics, meaning they’re created from living cells. Other DMTs are synthetic. Both work by interrupting the chain reaction that causes inflammation and the immune system response. The different drugs disrupt the inflammation cascade at different points and with varying effectiveness—but the result is less damage to myelin and fewer relapses.
In fact, these medications have been shown in clinical trials to reduce the severity and frequency of relapses, reduce the number of lesions in the brain and spinal cord, and slow the progression of disability for many people with MS. They’ve also been shown to be most effective when people with MS adhere to a doctor’s instructions and take them as directed.
The American Academy of Neurology (AAN) has created guidelines for stopping disease-modifying medications—don’t ever do this on your own. Some of these DMTs may cause serious side effects. Talk to your doctor about how you’re feeling, and together you’ll come up with the right disease-modifying therapy approach for you.
Disease-modifying therapies include:
Injectable medications (administered via needle, self-injected daily or a few times a week), like Avonex and Rebif (interferon beta 1a); Betaseron and Extavia (interferon beta 1b); and others.
Oral medications (taken by mouth once or twice a day), like Aubagio (teriflunimide), Gilenya (fingolimod), Zeposia (ozanimod), and others
Infused medications (administered intravenously a few times a year), like Campath, Lemtrada, and MabCampath (alemtuzumab), Novantrone (mitroxantrone), Ocrevus (ocralizumab), and more
There are fewer choices for treating the more progressive form of the disease (SPMS), because damage to the CNS is more widespread. DMTs that can treat SPMS include:
Mavenclad (cladrabine)
Betaseron (interferon beta 1b)
Novantrone (mitoxantrone)
Mayzent (siponimod)
Corticosteriods
To treat severe inflammation during a relapse, your doctor may also give you a high dose of oral or intravenous corticosteroids.
In the short-term, corticosteroids can be quite effective because they repress your immune response—which stops your body from attacking its own tissues, causing inflammation and demyelination. However, they show no long-term benefit to other MS symptoms, and they can deliver a wide range of side effects over the long-term, including high blood pressure (HBP), bone loss, and high blood sugar, all of which negatively impact your health. So, if you get them, you’ll likely only receive corticosteroids for a short period of time during an attack.
You may also have other symptoms of MS to manage with medications, too, including bladder and bowel dysfunction, fatigue, tremors, spasticity, walking (gait) difficulties, sexual problems, itching, nerve pain, depression, and/or dizziness and vertigo. Depending on your specific set of symptoms, your doctor (or doctors) will prescribe the right combination of drugs for you.
Your MS Team
Which brings us to your MS medical team—because if you have MS, you’ll almost certainly be treated by not just one specialist but by many who will manage your physical and emotional health. This team mostly likely will be led by a neurologist. Depending on your specific symptoms and disease course, you might also see:
Neuropsychologists to manage cognitive and emotional symptoms
Urologists to treat bladder dysfunction
Physical therapists to manage movement symptoms
Ophthalmologists to treat optic neuritis
Social workers to connect patients to resources

Living With MS
We’ve all heard how important it is for us to take good care of our health—eating well, exercising, getting quality sleep, seeking strong emotional support systems—yet it’s doubly important for someone with MS. That’s because research shows how your everyday choices, from what you eat to how much you move and sleep, to how well you cope with stress, can actually affect the disease progression of MS.
The first, most important thing you can do is to manage your MS to the best of your ability. That means paying attention to, and seeking treatment for, all your symptoms, preferably in their earliest stages by following your doctors’ instructions, and by signing up for ongoing rehabilitation to promote mobility, cognitive function, and social connection.
So, let’s start with the basics about your lifestyle—and what they mean for someone with MS.
Diet and Nutrition
There is no dedicated MS diet. But certain foods—and drinks—are known to promote inflammation in the body. And if you have MS, inflammation is what you want to avoid, at all costs. A good basic guide? Follow the tenets of the Mediterranean diet, which is big on olive oil and fatty fish (packed with inflammation-fighting omega-3 fatty acids); lots of colorful fruits and veggies; and plenty of whole grains. Also smart: Make sure you’re getting enough low-fat dairy. You need 1,000 to 1,500 mg of calcium a day to stave off bone loss, which is common among people with MS.
Things worth avoiding (or at least limiting): Added sugars, which fuel inflammation; extra caffeine (a cup or two in the morning is fine, but more can aggravate bladder and sleep issues); and salt (high levels of sodium have been linked to flares).
Exercise
Exercise is essential to MS management, largely because it, yep, actively combats symptoms of this disease. In fact, research shows it can preserve brain tissue and function, build strength, and improve balance and coordination. It can also improve overall quality of life—more energy, mental focus, and a boost of happy brain endorphins, too, which you’ll welcome if you’re living with a chronic condition.
And while the thought of working up a sweat—or even just moving off the couch on some days—may feel like an insurmountable task, it’s so, so very important that you try. Having said that, every person with MS is different, so speak to your doctor before you begin any exercise program, and when you’re ready, consider starting out with a trainer or physical therapist who regularly works with MS patients.
Cognition
What we really mean here is exercising your mind. Cognitive decline can be a big issue for people with MS—65% of people with this condition report experiencing trouble focusing, processing information, and struggling with memory—but there are ways to help combat it. That’s because the human brain is not static. It uses what is called our cognitive reserve—everybody has this backup system, not just people with MS—to form new connections, and to change and adapt. However, this reserve is not unlimited—it can only do so much. So help your brain health by doing any and all of the following:
Read more: Reading stimulates many parts of the brain—which is good for yours!
Get lost in thought: Doing puzzles, playing memory games, learning a new language, or even balancing your checkbook in your head all help fight cognitive decline. Even engaging in fun hobbies like doing artwork or journaling count.
Be social: Join a book club (reading!). Work out with a friend. Attend a church gathering or support a cause or foundation that speaks to your specific interests. When we’re social, we’re engaging our brains in many different ways, including the parts responsible for attention, language comprehension, and working memory.
Sleep
If you’re living with MS, sleep is essential—maybe more for you than for most people, and for so many reasons. And because of your condition, it may be harder to come by quality, consistent Zzzs. Problems with insomnia, spasticity, stress, nerve pain, and depression can all contribute to your not getting enough shuteye—even when shuteye is exactly what you need most to combat the crippling fatigue that comes with a disease flare (and sometimes outside of one).
Other Things to Keep in Mind
Monitor your cardiovascular health. Heart problems often coincide with MS. Remember, that inflammation that’s causing your symptoms can affect every cell in your body, including your heart. This is another reason why exercise matters so much. So work with your doc to keep close tabs on your heart health.
Manage stress. Stress certainly doesn’t help your MS symptoms. In fact, it can even cause additional symptoms to emerge. Try talking to a therapist, practicing mindfulness, exercising, or joining a support group to keep your stress at bay.
Take sex seriously. Don’t ignore your sex life, even if your MS symptoms are making it a little trickier. There are treatments available to make sure you can still have a normal sex life–talk to your doc to get more info.
Keep your pregnancy plans (if you have them!). There is no evidence that MS impairs fertility, so you need to take all the precautions anyone else would if you’d rather not start a family at this time. If, however, you ARE ready to conceive, you’ll need to consider a few things before going for it, such as any disease-modifying medications you might be taking right now. None are currently approved as safe to use during pregnancy by the FDA, which also recommends that you stop using them prior to conception. Be sure to talk with your doctor for guidance if you wish to start a family.
Where Can I Find My MS Communities?
People with MS sometimes feel isolated, since their symptoms can literally take them out of the game, trip them up, or all but beg them to head back to bed. Try not to let MS limit your life—or shut you off from the people, places, and activities you enjoy. For inspiration, we’ve put together a social list to help you stay connected and (way) less alone:
Top MS Instagrammers/Bloggers to Follow
Randy Patrick, @must_stop_ms and MustStopMS on Facebook
Follow because: This is your weekly social roundtable to talk all things MS—including the personal stuff that you wouldn’t normally talk about—but there’s something about Randy and the #ChatMS platform (found weekly on Facebook and Twitter) that brings it out in you.
Aaron Boster, M.D., Multiple Sclerosis on YouTube
Follow because: He’s not only a highly respected MS neurologist, but he talks about MS on a patient level—as in, you can actually understand what he’s saying. His passion for sharing his insight about MS comes across as both informative and entertaining.
Selma Blair, @selmablair
Follow because: If you don’t already know her, you need to. Selma isn’t just a name because she’s a well-known actress, appearing in movies like “Cruel Intentions” and “Legally Blonde,” she’s also increasingly becoming the most real, raw, and outspoken MS advocate out there. Whether she’s letting her kid cut her hair (which she started shedding due to MS), or rocking the coolest cane, she is no doubt going to inspire you and make you feel stronger, just by scrolling her feed.
Trevor Wicken, @themsgym and themsgym.com
Follow because: Not your average exercise-inspo—these are specifically tailored workouts (including videos) that teach people how to use neuro-muscular exercise and mindset to help them transform their lives. Not only do you get the perks of Trevor’s MS-friendly sweat sessions, but you join a community of people just like you, trying to work their joints and their brains.
Dave Bexfield, @activemsers
Follow because: It’s the perfect mix of living (and we do mean living—across the globe, even) with MS and sharing evidence-backed research on diet and exercise, plus how he implements these tips into his life, with some natural inspiration as to why you should, too.
Ardra Shephard, @ms_trippingonair
Follow because: Her motto is “trip through life without wrecking the pretty”—if that’s not reason enough to follow her, maybe her sense of humor (and how she blings-out a mobility device) will entice you.
Top MS Podcasts
FUMS Now. Hosted by Kathy Reagan Young, who combines humor and attitude to tell the “MonSter” to shove off while providing practical information and tips for living better with the disease.
RealTalk MS. A place where everybody knows MS. Jon Strum brings together neuroscientists and MS clinicians to share the latest news and breakthroughs in MS, but softens the research-heavy talk with inspiring stories of individuals who are doing remarkable things in the MS community.
Overcoming MS. It’s not just about the medication and treatments that provide a chance at living a “normal” life with MS, it’s also about your lifestyle. That’s why Geoff Allix brings in scientists and fitness and nutrition experts to help you modify your lifestyle for a chance at living your best life with MS.
Need to Know with Sam and John. Hosted by two friends—John Platt and Samantha Villella—who are navigating the world of MS together, then sharing their experiences with the rest of the world. They dive in to the off-the-wall topics that the MS community craves but doesn’t always get the chance to talk about.
MS Organizations and Non-profits
National MS Society. Their vision? A world free of MS. While they help to raise awareness to work towards that, they provide people affected by MS with the resources needed to restore what has been lost and create a new normal.
Live Wise MS. This is a unique resource for people living with MS, featuring posts from the MS community, plus information culled from a wide variety of resources that’s turned into a search tools on their website where you can look up symptoms and management tips.
MS Foundation. Known in the MS community as MS Focus, this nonprofit provides free services that address the critical needs of people with MS and their families, helping them maintain the best quality of life possible.
MS Association of America. This national non-profit also offers free programs to improve the lives of folks with MS and the families who love them, providing online chatting with trained specialists, MS equipment and accessories (like cooling vests), educational programs, peer-to-peer forums, and more.
No, you won’t die from MS, itself. Studies do suggest that people with MS are at increased risk of dying earlier from complications such as heart disease, diabetes, infection, pneumonia, and other conditions, so it’s important to be monitored by a medical team. Which you will be. And they'll do everything they can to help you stay as healthy as possible.
MS isn’t passed down from generation to generation, but the susceptibility for the condition might be. People who have family members with MS are at increased risk of developing it, too, and researchers have identified more than 230 genes associated with increased MS risk.
Women are more likely than men to have most types of MS. The most common type of multiple sclerosis—relapsing-remitting MS, accounting for up to 85% of MS cases—affects women two to three times more often than it does men. Men and women have an equal risk for primary-progressive MS, the much rarer form.
Not yet, but the progress made toward a cure in the last two-and-a-half decades has been astounding. Quality of life for people with MS is much higher than even 10 years ago, and scientists know more about the causes of MS than ever before.