Depression: Everything You Need to Know
We've got the doctor-approved details on depression causes, symptoms, treatments, and a jillion other tips that can make life with depression a little bit easier—and hopefully, eventually, happier.






How are you feeling today? If you’ve found yourself reading this, probably less than awesome. Maybe you’ve been feeling listless and down for a lot longer than you expected, and it’s making you worry that you might have depression. Maybe you’ve just received a diagnosis of clinical depression and you’re looking for answers. We get it. So many contributors to HealthCentral have felt just like you do now. But we won’t let depression swallow you up. We also won’t bombard you with a bunch of false promises and inaccurate information (that’s what your Facebook feed is for). Here, we share the reality of coping with depression, as well as expert advice from top doctors, the most successful treatments, and mood-lifting lifestyle changes.
What Is Depression?
It’s normal to experience sadness. (Who didn’t cry when Simba couldn’t wake up Mufasa?) But unlike typical sadness or grief, time can’t and won’t heal Major Depressive Disorder (MDD), the term for clinical depression, which most people just call “depression.” It’s a common mental health condition that shows up like an unwanted houseguest and refuses to leave. This extended period of sadness or emptiness comes with a constellation of other symptoms, like exhaustion, sleep trouble, a shrinking appetite, overeating, sudden crying spells, and sometimes thoughts of suicide. Symptoms range in severity and must last for two weeks or more to receive an MDD diagnosis, though it’s rare that an episode would only last for that short time. Most people have symptoms for six months to a year, and sometimes, they can last for years.
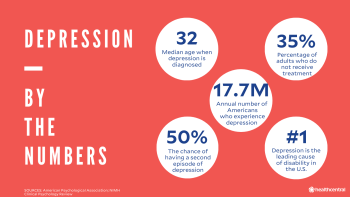
Without treatment, depression won’t fade away on its own. Even if you do white-knuckle it through your first episode of depression, your chance of another recurrence is more than 50 percent. Meaning, you’re going to want to deal with this sooner rather than later.
One hallmark of depression is an inability to experience pleasure, which is literally no fun. Losing interest in things you once enjoyed often means that your capacity to function at work and home takes a dive. In fact, depression is one of the leading causes of disability in the U.S., as 7.2% of Americans—17.7 million people—experience major depressive disorder, each year.
How Common Is Depression?
Major depression is one of the most common mental illnesses in the country. An estimated 17.3 million adults in the US reported having at least one major depressive episode over the course of a year, a 2017 report by the Substance Abuse and Mental Health Services Administration (SAMHSA) shows. Women have a higher prevalence of experiencing a major depressive episode than men (8.7% compared to 5.3% for adult males).
Depression is especially crushing for the workforce: It’s the number one leading cause of disability worldwide, according to the World Health Organization. The total economic burden of MDD is estimated to be $210.5 billion per year in the United States alone—a figure that reflects costs associated with missed days, reduced productivity, treatment for depression, and suicide.
Types of Depression
We talked about MDD (a.k.a. depression) but there are other types of depression. Depression of all types strikes people at a median age of 32, but it's important to remember that it can happen to anyone, at any age, race, or gender. One out of every six adults will experience depression at some time in their life. Fortunately, depression is treatable. That’s why, at the first hint of symptoms, it’s important to make an appointment with a mental health professional who can help determine whether you have depression, and if so, which type—which helps inform which treatment is appropriate for you. The different types of depression include:
Persistent Depressive Disorder
This is a chronic form of depression, formerly known as dysthymia. Sometimes people call it “high functioning” or “smiling” depression. While symptoms aren’t as severe as MDD, they last for two years or longer. People with PDD might feel like they’ve always been depressed. (In cases of “double depression,” people experience severe episodes of MDD within their usual state of chronic depression.)
Seasonal Affective Disorder (SAD)
Depression symptoms start and end seasonally, around the same times every year. Most people get depressed in cold, dark winter, but some people’s mood plummets in summer.
Premenstrual Dysphoric Disorder (PMDD)
Here, depression symptoms are tied to the luteal phase of the menstrual cycle (so, it goes without saying, but this type only happens in those who menstruate), starting about one week before your period and ending just after your period. Though many of the symptoms mirror PMS,they’re much more severe and are essentially like a depression relapse, coming and going with the monthly menstrual cycle. They interrupt your ability to work, destroy personal relationships, and can lead to thoughts of self-harm and suicide. This condition was added in 2013 as a form of depression to the DSM-5, the official guide of mental disorders.
Peripartum Depression
New mothers with this disorder typically develop symptoms of depression and even psychosis (a rarer occurrence) within a few weeks of giving birth. It used to be called postpartum depression and many people still use the term interchangeably. This type can happen before a baby is born, or prenatal depression, and after, or postpartum depression (hence the name change), with a stunning 1-in-9 new mothers experiencing after-birth this type.
Perimenopausal Depression
In their 40s (the average of menopause is 51), people assigned female at birth can experience this depression type plus perimenopause symptoms like hot flashes and night sweats.
Substance/Medication-Induced Depressive Disorder
Substance abuse (alcohol, opiates, sedatives, amphetamines, cocaine, hallucinogens, etc.) or taking some medications, like corticosteroids or statins, can trigger the symptoms of depression. If substance use (or withdrawal from using) is causing your symptoms, you may have this version of depression.
Disruptive Mood Regulation Disorder
A child with this juvenile disorder is grumpy and bad-tempered most of the time. They have severe, explosive outbursts with parents, teachers, and peers several times a week. Their overreactions are extreme and inconsistent with their developmental level.
Depression and Other Disorders
Turns out, depression can also happen in concert with other mental health conditions. Such as bipolar and depression. Bipolar disorder, which used to be called manic depression, is a mental health condition that has cycles of high energy/emotion (called mania or hypomania) and low energy/emotion (or depression).
Or depression and anxiety. They’re separate conditions, but commonly happen together in several ways. Like, anxiety might be a symptom of MDD, or you might have depression caused by an anxiety disorder (like generalized anxiety disorder, panic disorder, or separation anxiety disorder). You can be diagnosed with both or just one.
Another common combination is depression and OCD, or obsessive-compulsive disorder. Researchers estimate that one quarter to one half of people with OCD (which totals some 2.2 million adults in the U.S.) also meet the diagnostic criteria for a major depressive episode. It seems that depression occurs most often because of the “distress and devastation” of OCD, a condition where you have excessive thoughts, or obsessions, that then cause repetitive behaviors, or compulsions. But some people experience onset of both at the same time (or have depression before OCD).
Or you might have depression and psychosis. Officially called psychotic depression (or depression with psychosis), numbers vary about how frequently this happens, from 14% to nearly 50% of those diagnosed with depression having it (older patients are more likely to have it as well). This psychosis is considered a transient mental state where people who are depressed might also experience delusions (which are more common) and hallucinations (which are less common). Delusions are the belief in something that’s not real, while hallucinations hear voices or sees things that are not real. This sounds scary, we know, but the treatment prognosis is excellent.
Depression Causes
So what makes depression happen? The truth? No one knows for sure what causes depression. For the past few decades, the prevailing theory is that depressed people have an imbalance in their brain chemistry—more specifically, low levels of neurotransmitters like norepinephrine, epinephrine, and dopamine, which help regulate mood, sleep, and metabolism. We now know it's a little more complicated than that.
Certain circumstances put people at a higher risk of depression, including childhood trauma, other types of mental illness and chronic pain conditions, or a family history of depression, but anyone can get depressed.
Scientists informed by decades of research believe that the following factors also up your risk of becoming depressed, but they can’t prove causality. Still, they can play heavily in the development of depression, so it’s important to be aware of them:
Family History
Research shows that having a first-degree relative with depression (a parent, sibling, or child) makes you two-to-three times more likely to have depression tendencies, so genetics could play a key role.
Traumatic Life Events
Everyone goes through rough patches in life, and for some people, the patches are rougher and their response is more severe. Traumatic life events, especially those from childhood such as abuse or neglect, are risk factors.
Environmental Stressors
Things in your everyday life, including a loved one’s death, a messy divorce, or financial problems, are all potential risk factors for developing depression. So, too, are environmental stressors like losing your job, having an unpredictable boss, or even working shift hours.
Medical Conditions
Such as underactive thyroid or chronic pain). Per science, the relationship between these physical conditions and depression is bidirectional, so there’s a chicken-or-egg thing going on because they feed each other. In addition, certain medications used to treat condition, like sedatives and blood pressure pills, may raise your risk for depression.
Hormonal Changes
A shift in your natural hormone levels can trigger a bout of depression. This can occur for any number of reasons and is also a normal part of the life cycle for both women and men. For instance, hormone levels change with both childbirth and menopause.
Gut Bacteria
There has been a link established between the microbiome and the gut-brain axis, but it’s only just starting to be studied.
Drug Use
Chronic use of recreational drugs can cause changes to the brain structure, leading to mental health issues like depression.
Do I Have the Symptoms and Signs of Depression?
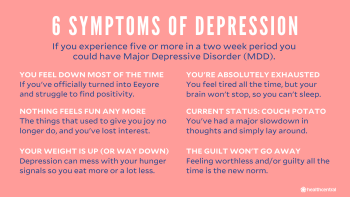
Wondering whether your feelings qualify for clinical depression? Those with MDD experience five or more of the below symptoms of depression during the same two-week period, and at least one must be depressed mood or loss of pleasure. The symptoms and signs of depression would be distressing or affect daily functioning.
You feel down most of the time.
The things you liked doing no longer give you joy.
Significant weight loss (without dieting) or weight gain or feeling consistently much less hungry or hungrier than usual.
Having a hard time getting to sleep and staying asleep or oversleeping.
A molasses-like slowdown of thought, becoming a couch potato, or spending days in bed. (This should be noticeable to others, not just subjective feelings of restlessness or slothiness.)
So. So. Tired. You’re so exhausted you can’t even.
Feeling worthless a lot of the time, even if you haven’t done anything wrong.
Being super distracted, indecisive, and unable to concentrate.
Recurrent thoughts of death or suicide (with or without a specific plan to actually do it). If you need help for yourself or someone else, please contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
Symptoms and signs of depression can differ by gender and what age you are, too. Here are some of those ways:
Men and Depression
According to the National Institute of Mental Health, men will sometimes hide their depression, and whereas women might be sad when they are depressed (as we commonly think of depression being) and more willing to discuss their emotions and feelings, men might not be so open. As a result, they might experience depression symptoms as:
Anger, irritability, aggression.
Feeling anxious, restless, on edge.
Losing interest in work, family, or hobbies.
Experiencing issues with sexual desire and performance.
Engaging in high-risk activities.
A strong need for alcohol or drugs.
Physical aches or pains that can include headaches, cramps, or digestive problems.
Thinking about, or attempting, suicide.
Women and Depression
While women can have depression with similar symptoms to men—like irritability, aches and pains and digestive problems, and considering suicide—they have their own symptoms too, including:
Persistent sad, anxious, or “empty” mood.
Feeling hopelessness or pessimistic.
Feeling guilty, worthless, or helpless.
Decreased energy.
Moving or talking more slowly.
Feeling restless or having trouble sitting still.
Women can also be depressed at specific points in their life unique to their experiences, including: Premenstrual Dysphoric Disorder (PMDD). Symptoms include irritability, anger, depressed mood, sadness, suicidal thoughts, and appetite change as some of its symptoms. Perinatal Depression. Symptoms can include extreme sadness, anxiety, and fatigue. Perimenopausal Depression. Specific symptoms are irritability, anxiety, sadness, or loss of enjoyment.
College Students and Depression
Being in college can be an exciting time, as both men and women embark on their first forays into the world as young adults. It can also be an overwhelming time of challenging new experiences, including living on their own for the first time, tough school work, financial concerns, navigating relationships, balancing work and school. So it’s no surprise that 30 percent of college students felt “so depressed that it was difficult to function” sometime in the last year, according to a nationwide 2011 survey conducted by the American College Health Association–National College Health Assessment (ACHA–NCHA).
Students need to know the above info, that depression symptoms can differ between men and women. They also need to be aware of just what’s at stake: The third leading cause of death for teens and young adults ages 15 to 24 is suicide. And in that ACHA–NCHA survey, more than 6 percent of college students reported seriously considering suicide; about 1 percent reported attempting suicide in the previous year. Receiving help is vital. On-campus mental health services including counseling centers, student health centers, a trusted professor or student advisor, or doctor might assist with care.
Other key pieces of info for this age group and depression:
Research suggests that college students with depression are more likely to smoke.
Depressed college students (especially women), are more likely to “drink to get drunk and experience problems related to alcohol abuse, such as engaging in unsafe sex,” according to the National Institute of Mental Health.
Teens and Depression
With the hormonal roller coaster ride of puberty can come a feeling of sadness that lasts for weeks or months. It can happen in both boy and girl adolescents. Symptoms can include:
Sadness.
Feeling empty or hopeless.
Being angry, irritable, or frustrated (even at little things).
Having no joy in things you once loved.
Losing weight when not dieting or gaining weight from eating too much.
Having trouble falling asleep or staying asleep, or sleeping much more than usual.
Feeling restless or having trouble sitting still.
Feeling very tired or not having energy.
Feeling guilty or worthless.
Having trouble concentrating, remembering information, or making decisions.
Thinking about dying or suicide. (We can’t say it enough--please contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).)
Children and Depression
You might not associate depression with kids, but it can happen. According to the Centers for Disease Control and Prevention, 3.2% of children ages 3-17 years old, or approximately 1.9 million, have been diagnosed with depression. Keeping in mind the state that suicide is among the leading cause of death in 10-24 year olds, knowing the symptoms can save lives. For children, they include:
Feeling sad, hopeless, or irritable a lot of the time.
Not wanting to do, or enjoy doing, fun things.
Eating considerably more or less than usual.
Sleeping much more or less than normal
Being tired and sluggish or tense and restless a lot of the time.
Struggling to pay attention.
Feeling worthless, useless, or guilty.
Showing self-injury and self-destructive behavior.
How Do Doctors Diagnose Depression?
When you’re having a depressive episode, it might feel like you’re destined to feel terrible forever. That’s not true. It’s just what your depressed brain wants you to think. The hardest step is ignoring that feeling and making an appointment with a doctor and/or mental health professional, such as a psychologist or psychiatrist. A mental health professional is the only expert that can help you figure out if you are depressed.
Unfortunately, there’s no easy blood test that can determine if you have depression, though that would make diagnosis a lot easier. (Get on it, science!) The DSM-5 helps clinicians make that call with a targeted list of common symptoms. To be diagnosed with MDD, patients must experience five or more of the above symptoms (see “Do I Have the Symptoms of Depression?”)—one must be in a depressed mood or have a loss of pleasure—during a two-week period.
Even if your symptoms match up to MDD, though, your doctor should rule out any underlying medical causes first. Some conditions, such as thyroid disease and vitamin deficiency, can mimic symptoms of depression. Next, consider any medications you’re currently taking.
If this sounds like you or someone you know, make an appointment with a mental health professional. Now. Don't wait! What's the worst thing that can happen? If you feel better by the time the appointment rolls around, you can always cancel it. If you don’t, you’ve saved yourself precious time (and unnecessary pain) by taking steps to managing your mental health.
Depression Tests
Even though there’s no one laboratory test that can definitively say, you have depression and how severe it is, there are rated questionnaires that can help your healthcare professional determine your level of depression. These include:
Beck Depression Inventory. This 21-item, self-reported questionnaire takes about 10 minutes to take, and provides mental health professionals with info to help determine your symptoms of depression. It’s been around awhile (and updated multiple times)—since its publication in 1961 in Archives Of General Psychiatry (now JAMA Psychiatry).
The Hamilton Depression Rating Scale (HDRS, Ham-D). Another 21-item, self-reported questionnaire (which takes about 20-30 minutes to administer), this one helps mental health professionals determine the level of depression, and any change, in symptoms after diagnosis. A higher score likely means more severe depression. Also a much older tool (first published with 17 questions in 1960 in Journal of Neurology, Neurosurgery, and Psychiatry), it’s also the most widely used clinician-administered depression assessment scale.
Treatment for Depression
Regardless of why you’re depressed, it’s important to get treatment before the condition starts to erode your quality of life. Studies and surveys show that most adults in the U.S. who screen positive for depression remain untreated. Don’t be one of them.
As scientists continue to hash out theories about the root causes of depression, research shows that the most effective treatment is a mix of psychotherapy, medication, and lifestyle changes. It might take a (frustratingly long) while to find the right recipe—antidepressants work differently in different people so finding the right fit often takes some trial and error. Plus, the mental health professional you’re working with will be by your side. They won’t give up and neither should you. Some of the treatment options available are:
Psychological Counseling
There are multiple different types of therapy that can help with depression. We’ll touch on three popular types, but know there are more that you might explore with your mental health professional. This all doesn’t mean you’ll find yourself reclined on a couch, complaining about your relationship with your mother (though it might). The following healthcare professionals can help you with this treatment:
Psychiatrist
Psychologist
Therapist
Licensed clinical social worker
They might use a variety of techniques to help change the negative thinking, beliefs, or behaviors that exacerbate your depression and make your world seem hopeless. Types of therapy include:
CBT for Depression
This treatment, called cognitive behavioral therapy or CBT for short, is one of the most “evidence-based psychological interventions” for depression, according to an article published in 2020 in the Indian Journal of Psychiatry. It’s basically talk therapy, a new way of learning how to think, behave, and approach life in a positive way by identifying and evaluating automatic thoughts that can lead to negative behavior/outcomes. The approach was developed by Aaron T. Beck, M.D., in the 1960s (yes, the same person who created the Beck Depression Inventory!), and it’s stood the test of time. It can be done on an out-patient basis, with regular planned sessions lasting about 45 minutes to an hour between patient and healthcare professional.
Interpersonal Therapy for Depression
This time-structured treatment approach, typically done as individual therapy sessions or group work in 12 to 16 weeks, was developed only about two decades ago as a research intervention for major depression disorder, but has gained popularity in recent years with clinicians (i.e., practicing mental health professionals). It seeks to change relationship patterns and difficulties instead of associated depression symptoms with a focus on interpersonal relationships (hence its name).
Psychodynamic Therapy for Depression
One of the oldest forms of therapy today, going all the way back to Freudian psychology (paging Sigmund Freud), circa 1900, it uses awareness of how your subconscious can cause self-destructive behaviors to treat depression. These insights can direct how you approach different situations and navigate life. Research has shown that its an effective treatment for a variety of conditions, including depression.

Depression Medications
Your depression might require more than therapy, or therapy combined with medication.. Doctors may prescribe medication including:
SSRIs (Selective Serotonin Reuptake Inhibitors)
These meds, the most commonly prescribed antidepressants, work by increasing serotonin in the brain, blocking the reabsorption (or reuptake) of serotonin into neurons, which then makes more serotonin available. This allows better transmission of messages between neurons. The following meds are thought to work in similar ways, and have similar side effects (though sometimes switching meds within this class can stop those, so talk to your doctor if you’re experiencing any of the following). These can include nausea, increased appetite (leading to weight gain), headache, drowsiness, dry mouth, insomnia, nervousness, dizziness, and sexual issues (like decreased libido). Be sure to discuss other medications you take, any precautions specifically for you when starting a new med, how to stop SSRIs (they should be tapered so you don’t experience withdrawal symptoms), and any concerns about a raised risk of suicide taking these (and any other antidepressant meds).
Celexa (citalopram): This oral med is typically taken once daily by mouth, in the morning or evening, with or without food, and is often started at a lower dose and slowly increased over several weeks. Doses range from 10 mg to 40 mg. The brand name drug (Celexa) is available as a tablet, while the generic (just citalopram) is available as both a tablet and liquid.
Lexapro (escitalopram): This oral med is usually taken once a day with or without food. Doses range from from 10 mg to 20 mg, and are often started low and increased over several weeks. It can be a tablet (brand name) or tablet and liquid (generic).
Paxil, Pexeva, Brisdelle (paroxetine): Typically taken one time per day with or without food, this oral med is usually begun at a low dose and increased over time. When taken for PMDD, it can be taken daily or intermittently. Dosages go 10 mg to 40 mg (75 mg for controlled release). It can be taken as a tablet for immediate release (Paxil, Pexeva), controlled release, liquid (Paxil), and capsule (Brisdelle).
Prozac, Sarafem (fluoxetine): This oral med is usually taken one time per day with or without food but for PMDD, can be taken daily or intermittently. Dosages range from 20 mg to 80 mg when taken once daily or 90 mg taken once weekly, and are typically started low and increased. It’s available in different ways, including as a capsule (Prozac); delayed-release capsule (Prozac Weekly); tablet (Sarafem); and capsules, delayed-released capsule, liquid, tablet (the generic).
Zoloft (sertraline): This oral med is taken usually once a day with or without food, starts with a low dose, gradually increasing to a higher dose. Dosages range from 50 mg to 200 mg. For PMDD, it can be taken daily or intermittently. It can be taken as a tablet or liquid.
SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors)
These antidepressant meds cause brain chemistry and communication changes in the brain nerve cell circuitry, helping regulate mood and relieve depression. The most common side effects of this class of drugs are: Nausea, dry mouth, dizziness, headache, and excessive sweating. Other side effects can include loss of appetite, sexual problems, tiredness, constipation, and insomnia. Talk to your healthcare professional about what else you should know about these meds.
Pristiq, Khedezla (desvenlafaxine): This oral med is taken as an extended release tablet one time per day with or without food. The usual dosage ranges from 50 mg to 400 mg.
Cymbalta (duloxetine): This oral med is also approved to treat anxiety and certain types of chronic pain and is usually taken 1 or 2 times per day with or without food. The dosage ranges from 20 mg to 120 mg. It’s available as a delayed release capsule and the Drizalma Sprinkle version is a delayed release sprinkle capsule.
Fetzima (levomilnacipran): This oral med is taken as an extended release capsule, usually taken one time per day with or without food. The dose range is 20 mg to 120 mg.
Effexor, Effexor XR (venlafaxine): This oral drug can also treat certain anxiety disorders and panic disorder. It’s taken two ways: Immediate release tablets are usually taken two or three times per day with or without food, while extended release tablets and capsules are taken one time per day with or without food. Doses range from 37.5 mg to 300 mg.
TCAs (Tricyclic Antidepressants and Tetracyclic Antidepressants)
These meds, also called cyclic antidepressants, were among the first antidepressants created and work to affect the neurotransmitters that communicate with brain cells. They’re not used as often now as they were once because of unpleasant side effects. Potential common side effects are: drowsiness, blurred vision, constipation, dry mouth, blood pressure drop when moving from sitting to standing, urine retention. There are a number of generic drugs available in this class; we’ll cover three with brand names.
Tofranil/imipramine: An oral med in tablet form, it’s given in doses ranging from 75mg to 200 mg, usually once a day.
Norpramin/desipramine: An oral med also in tablet form, adults usually take 100 to 200 milligrams (mg) once a day or in divided doses during the day.
Nortriptyline/Pamelor: This oral med, which can be taken as a capsule or liquid, is often administered as 25 milligrams (mg) 3 to 4 times per day (and can be dosed up to 150 mg).
MAOIs (Monoamine Oxidase Inhibitors)
These effective meds were the first type of antidepressant developed, but they’ve fallen out of favor because of their side effect profile. They work by changing the brain chemistry involved in depression, but also affect other neurotransmitters in the brain and digestive system, which causes the side effect issues. They can include (but are not limited to): dry mouth, nausea, diarrhea or constipation, headache, drowsiness, insomnia, dizziness or lightheadedness, skin reaction at the patch site. You might need to avoid certain foods, drinks, and medications while taking these drugs, so be sure to discuss with your healthcare professional.
Emsam (selegiline): This is given in a transdermal route, meaning as a patch on your skin. It’s applied to the upper torso, so below the neck and above the waist, upper thigh, or the outer surface of the upper arm once every 24 hours. The dose range most effective in studies was 6 mg to 12 mg over a day.
Marplan (isocarboxazid): This oral med is a tablet given as one tablet (10 mg) twice daily and slowly increased to possibly 60 mg divided into two to four doses.
Nardil (phenelzine): This oral tablet is first usually given as 15 milligrams (mg) three times a day (for adults), not to typically exceed a dose of 90 mg a day.
Parnate (tranylcypromine): An oral tablet medication, it’s usually taken one to three times per day depending on dose with or without food. The dose can range from 10mg to 60mg.
Atypical Antidepressants and Atypical Antipsychotics
Atypical antidepressants don’t fit in with other antidepressants and work differently from each other, hence their name. Second-generation antipsychotics are “atypical” in that they affect dopamine and other neurotransmitters without the physical side effects, such as tics and tremors, that first-generation antipsychotics can cause. As a result, these meds can also have unique side effects, specific to their medication. Here are only a few of these drugs, but are names you might recognize:
Wellbutrin (bupropion): This oral medication has many brand names (including Zyban and Aplenzin) and is taken as a tablet in immediate release (IR), sustained release (SR), and extended release (XL) formulations, all of which have different frequencies and doses of taking them.
Remeron (mirtazapine): This oral medication has been associated with an increase in cholesterol and weight gain. It’s usually taken one time per day at bedtime as either a table or oral disintegrating tablet. It’s typical dosage is 15 mg to 45 mg.
Seroquel (quetiapine): This oral med tablet is mainly used to treat schizophrenia, but can be used as adjunctive treatment of major depressive disorder, or in combination with an antidepressant. It’s typically taken 1, 2, or 3 times per day with or without food in 100 mg to 800 mg doses.
Abilify (aripiprazole): This med, given in different ways, is mainly used for schizophrenia as well, but can also be used as adjunctive treatment for MDD. Dose and administration vary, so discuss the best way and dosage of the drug with your healthcare professional.
Ketamine
Spravatoe/esketamine. For severe, treatment-resistant depression, the FDA recently approved a new medication, esketamine, a nasal spray based on the party drug/anesthetic ketamine. Experts say it works by kicking up production of glutamate, a neurotransmitter that helps prompt the brain to form new neural connections.
Alternative Treatments For Depression
Along with talk therapy and medication, there are other approaches to treating depression that may help you feel better, including less-used approaches for people with treatment-resistant depression. Additional depression therapies may include:
Brain Stimulation
For treatment-resistant depression that doesn’t get better after psychotherapy and more than two classes of antidepressants (such SSRIs and TCAs), there are more hardcore options. Severe depression may warrant electroconvulsive therapy (ECT). Fear not—modern ECT is safe, performed under anesthesia, and much less aggressive than you see in the movies.
There is also repetitive transcranial magnetic stimulation (rTMS) which some docs refer to as “ECT Lite.” For severe depression, some people receive vagus nerve stimulation (VNS), a surgical implant that works kind of like a pacemaker, sending electric pulses to the brain.
Light Therapy
Sadness during seasonal depression (SAD) can be alleviated with melatonin-regulating light therapy, but having a light box might also help with some types of depression that don't occur seasonally, too, according to the Mayo Clinic. Be sure to talk to your healthcare professional about getting the right light box for you, and best practices for using it to alleviate depression symptoms.
Exercise
Research shows that lifestyle changes like incorporating exercise can amplify results of medication and therapy. Even if they aren’t foolproof mood-lifters, it never hurts to build a health-supportive routine. Getting out and walking, cycling, swimming, doing yoga, and even dancing can add up to the 150 minutes of moderate exercise that the CDC recommends might help with mental health disorders like MDD.
Alcohol and Depression
Not drinking alcohol is key to lessening depression symptoms over time and getting the best results with any medication that you take, which often require no drinking for best outcomes. Doing so can be hard however, so for more help and information on how, reach out to the Substance Abuse and Mental Health Services Administration’s (SAMHSA) National Helpline, 1-800-662-HELP (4357), (also known as the Treatment Referral Routing Service) or TTY: 1-800-487-4889. This service is a confidential, free, 24-hour-a-day, 365-day-a-year, place to find out more about mental and/or substance use disorders in English and Spanish.
Drugs Linked With Depression
This might go without saying, but you also might not be aware that some drug use, including chronic use of recreational and illegal substances, can cause or worsen depression symptoms. So stopping is key to treatment outcomes. These drugs can cause mental health problems, according to the National Institute on Drug Abuse:
Cocaine
Inhalants
Kratom
LSD
Marijuana
MDMA
Methamphetamine
PCP
Some prescription drugs
Steroids (appearance- and performance-enhancing drugs)
Natural Remedies for Depression
When you think of other therapies for depression, your mind might go right to things like vitamins and supplements. While the science is still out on some of these possibilities, we’d be neglectful not to mention them, because you’ve no doubt heard of them. Supplements and vitamins can be bought over the counter. It’s key to know that the U.S. Food and Drug Administration (FDA) doesn’t regulate dietary supplements like they do medications, so it’s a buyer-beware market. Ones that might benefit those with depression include:
St. John's Wort
Results on this plant found in the wild are mixed, with research showing it had a similar effect as a placebo (when you think an intervention will help, even if you’re not actually on it) in clinical trials for treating depression. But it can have unintended consequences, like weakening birth control pills (so you end up pregnant when you very much did not want to) or heart medication. It can also interact badly with some antidepressants, leading to a potentially life-threatening increase of serotonin. This is why it’s so important to tell your healthcare professionals about everything you take and use, whether a supplement or medication.
S-Adenosyl-L-Methionine (SAMe)
This naturally occurring compound in the body can also be taken as a supplement. Some studies have found a positive effect in treating depression, but according to the Mayo Clinic, they were often small, with few patients. It does appear to be safe, while causing some potential side effects like anxiety and digestive problems, but might interact with antidepressants, so be sure to discuss taking this with your healthcare professional before you start.
5-hydroxytryptophan (5-HTP)
A chemical that the body makes from tryptophan (an essential amino acid found in food), as a supplement, 5-HTP can help raise serotonin levels in the brain, according to Mt. Sinai. Of note, back in 1989, a contaminant called Peak X was found in tryptophan supplements and was linked to an outbreak of eosinophilic myalgia syndrome, a potentially fatal disorder. The FDA pulled the supplements from the market. The contaminant has been found since in 5-HTP supplements, so be sure to purchase it only from a reputable source. Meanwhile, preliminary research seems to suggest that 5-HTP may work as well as some antidepressant drugs for those with mild-to-moderate depression, but more study is needed.
Omega-3 Fatty Acids
Fish oil supplements are a great way to get omega-3 fatty acids, which have a key role in brain function and could help in the treatment of mild to moderate depression—but more research is still needed in this field.
Essential Oils
Aromatherapy, a popular complementary and alternative medicine intervention using essential oils, shows potential as an effective therapeutic option for depression symptoms, according to an article published in Evidence-Based Complementary and Alternative Medicine in 2017, but the quality of six of the 12 studies reviewed in the piece was low, according to researchers. They reported that research did show that lavender, bergamot, and sandalwood improved depressive symptoms. More study is needed in this field as well, including in determining the best way of administering the oils and other details.
Vitamin B
A 2016 study provided evidence that vitamin B contributes to the complexity of depressive symptoms. Vitamin B1, B3, B6, B9, and B12 deficiencies have been linked to depression, researchers report. Vitamin B12 in particular is important, and has been associated with depression—and this vitamin isn’t made in the body but instead needs to be eaten in food or taken in a supplement. So should you start taking this vitamin to help with depression? First, consult with your healthcare professional before starting any new vitamin regime.
Vitamin D
It’s an important vitamin all around for your body, and research has shown a relationship between vitamin D deficiency and symptoms of depression. But researchers don’t know if low vitamin D levels are the cause OR the effect of depression. And vitamin D is one of many factors that may contribute to depression, making it hard to pinpoint its exact role or how important a role it plays. But one study, published in Neuropsychiatry in 2017, concludes that eating vitamin D-rich food, taking vitamin D supplements, and spending time in the sun might help with overall well-being if you have depression, so go for it. Be careful not to take in too much vitamin D in supplementation, however (which can happen)—your doctor can check your vitamin D level to determine if you need more supplementation or less.
Depression Prevention
Preventing bad outcomes with depression is vital work, and it’s important to know where you (or a loved one) can turn for help. Here are some places.
Samaritans
The Samaritans’ 24/7 Helpline, available in 240 languages and via a tele-interpreter service, is available if you’re depressed, lonely, suicidal, or just need to talk to someone, now. Call (877) 870-4673.
National Suicide Prevention Lifeline
The National Suicide Prevention Lifeline is a 24 hour, 7 days a week, free (and confidential) hotline. You don’t have to be suicidal to call. If you (or someone you love) are having a mental healt crisis, pick up the phone and dial this number: 1-800-273-8255 or 800-SUICIDE (hearing impaired – 800-799-4TTY) (Spanish 888-628-9454). Check out the Lifeline website, too.
Lifeline Chat
Speaking of the Lifeline website, check out the hotline’s Lifeline Chat, a service of the National Suicide Prevention Lifeline. It connects individuals with counselors for emotional support and other services through a free (and also confidential) web chat. Go here to find it.
Where Can I Find Depression-Related Communities?
The thing about depression is that it makes you want to roll yourself into a blanket burrito and never come out. But shutting out the world can make an already-bad situation worse by giving you free reign to neglect your needs, ruminate over your perceived flaws, and destroy any chance of forward momentum. Along with therapy and medication, finding supportive people—and connecting with them online and in real life—is a key part of taking care of yourself. Here's where to start.
Top Depression Instagrammers and Bloggers
Tonya Ingram, @tonyainstagram, tonyaingram.com
Follow because: She has one hell of a way with words—after all, she is a poet and author. She also battles some pretty heavy stuff like depression, lives as a “lupus legend” (her words—we love) and is currently waiting on the sidelines for a kidney transplant. She takes it all day by day and shares how she gets out of bed, looks herself in the mirror, and figures out how to simply... survive.
Scott Ste Marie, @depressiontoexpression, depressiontoexpression.com
Follow because: Immediately, he sounds like someone you want to be friends with, someone whose vibe you want to channel. A former Twitter employee and now public speaker, Scott isn’t going to guide you on some path to a complete cure—nor is he going to sugarcoat the realities of living with depression. In order to overcome your demons, Scott believes you have to come to terms with the fact that sometimes life sucks, and that’s okay.
Kevin Hines, @kevinhinesstory, kevinhinesstory.com
Follow because: You know the saying “What doesn’t kill you only makes you stronger”? Kevin Hines is living proof. He is the only person ever to survive a suicide attempt from the Golden Gate Bridge. After a sea lion kept him afloat, he was reborn as someone who now devotes his life to making sure you’re here tomorrow—which is why he regularly uses the hashtag #beheretomorrow.
Lola, Gina, and Nora Tash, and Nicole Argiris, @mytherapistsays, mytherapistsays.ca
Follow because: Sometimes the only way to come out of a deep dark hole is with the universal language of laughter. These girls (mostly family or like family) create endless hilarious memes that represent the real trials and tribulations of living in today’s social media-infested world. The point of it all? So you know that, as they put it, “you’re never alone and never as batshit as you think.”
Sad Girls Club, @sadgirlsclub
Follow because: It’s not your typical reel of inspirational quotes and nod-worthy memes — though, those are sprinkled in, too. Mostly, this feed—run by women of color (including founder @elyse.fox)—gives you actual advice on how to cope with depression, especially in modern-day situations, like discussing mental health at work (hashtag awkward). This feed gives you the ammo you need to shut down stigma.
Kate Allan, @thelatestkate
Follow because: Animals make everything better — especially when they’re paired with a quirky drawing and an all-too-familiar feeling. A wolf that speaks to your soul; a fox that gives you all the feels; and a bird who tells it like it is. Run by artist, author, and anxious human Kate, this page (and the cute animals that live there) is a feel-good must-follow.
The Sad Ghost Club, @theofficialsadghostclub, thesadghostclub.com
Follow because: Nathan, Lize, and Helen are besties—or, ghosties, as they refer to themselves—who came together to share life with mental illness from behind the computer screen. These ghosts don’t sugarcoat things, but they’re also not gloom and doom. You’ll be hooked on their graphics and positive (but not overly earnest) messages.
Top Depression-Related Podcasts
The Hilarious World of Depression. Stand-up comedy meets a psych appointment when actors and comedians struggling with depression tell their (surprisingly funny) mental health stories to “professionally depressed” host John Moe.
Terrible, Thanks for Asking. Author Nora McInerny, who has dealt with depression, isn’t afraid to ask the awkward questions, as real listeners share their own tales of coping with grief, despair, and anxiety.
Jen Gotch is OK...Sometimes. Ladyboss CEO and ban.do founder Jen Gotch gets vulnerable and real every week, sharing her struggles with mental health.
Anthologies of Hope. You’re here, and you’re reading this, so that in itself proves that you haven’t given up hope. But it’s not just that you are here—it’s why you’re here. This podcast dives even deeper into that “why” and tries to bring that to the forefront of your mind instead of the other garbage trying to pull you down. Host Rick Osowski, who has battled depression, brings a variety of guests into the fold to talk about their why.
Top Depression Support Groups and Non-Profits
Anxiety and Depression Association of America (ADAA). This nonprofit is dedicated to the prevention, treatment, and cure of anxiety, depression, OCD, PTSD, and co-occurring disorders. Come here for new research, monthly webinars from mental health experts, educational infographics and stats, and a Find-a-Therapist database you can search by disorder. You can always find (free) support on the ADAA Online Peer-to-Peer Support Group or support group iOS app for iPhone.
National Alliance on Mental Illness (NAMI). This nonprofit mental health advocacy group offering free education and support programs such as NAMI Peer-to-Peer (eight free sessions for adults with specific mental health conditions). You can also connect with other folks who have depression on this org’s online message boards and via NAMI Connection (use the site to find a weekly or monthly recovery group near you).
Reddit, r/depression. Reddit is the hideously under-designed social website for anonymous users with a bad rep for attracting “incels” and “neckbeards.” The self-proclaimed “Front Page of the Internet” has memes, conspiracy theories, and thousands of communities called subreddits—and some of them are quite lovely. For example, the r/depression subreddit is over a decade old with more than half a million subscribers. In here, the vibe is all about empathy, support, and helpful feedback. (A recent study even found that visiting the subreddit caused a “positive emotion change” in users.)
Talkspace. More like “safe space.” It’s online, it’s private, and it’s “open” 24/7. Over 1 million people use Talkspace to get matched up with one of their 5,000+ licensed therapists and then message them...as much and as often as they’d like. There are different packages depending on your needs, but the instant feedback and comfort is pretty much priceless.
Sad Girls Club. This is a nonprofit, an online community, and an Instagram handle (see above) focused on the millennial and Gen Z experience of mental illness (depression, anxiety, or something undiagnosed all count). They host meetups IRL where you can connect with similar people and try a cool twist on art therapy like a poetry slam or embroidery class.
To Write Love on Her Arms (TWLOHA). It’s not just a nonprofit — it’s a movement. Online, at in-person events, through social media and blogs, TWLOHA creates a place for hope and healing through depression, addiction, self-injury, and suicide. People who attend their events and join this community have said they’ve felt transformed. Worth a try, yea?
Sadness is a normal reaction to disappointment, bad news, and loss. (Remember when Jaime Lannister left Brienne of Tarth heartbroken to go canoodle with Cersei in King’s Landing?) Sadness and grief eventually let up over time, even after a devastating loss. Depression doesn’t go away, and it interferes with your ability to do what you need to do on a daily basis. Besides a gloomy mood, depressed people have other symptoms like fatigue, apathy, insomnia or too much sleep, noticeable weight change, crying jags, and (sometimes, but not always) thoughts of suicide.
To meet the clinical definition of a depressive episode, symptoms must last a minimum of two weeks (though research puts the median duration at six months). Chronic depression (aka Persistent Depressive Disorder) lasts a minimum of two years, but often lasts much longer. Depression can hang around forever, especially when left untreated.
That depends on the severity of your depression. Meeting with a therapist in person can be inconvenient, nerve-wracking, and just plain awkward. But is it really possible to text your way to better mental health? Experts are torn on the efficacy of virtual mental health apps (a.k.a. telepsychology). Research shows that text therapy like Talkspace, one-on-one chat, or video counseling makes getting help easier than ever, especially for super-busy people, those in rural areas where docs are scarce, or those who fear the stigma of being seen at a mental health office. Many experts caution against virtual therapy for people who are seriously mentally ill, have alcohol or drug addiction, or are at risk of harming themselves or others. In those scenarios, more intensive treatment is required. To find out how to get the most out of virtual therapy, check out the American Psychological Association’s guidelines for telepsychology.
Not necessarily. But they might. Suicide is the 10th leading cause of death in the U.S. for all age groups. Depression can wear on a person’s psyche, making every minute feel like an hour, stealing sleep, and creating a sense of hopelessness. We’re not trying to freak you out, but it’s important to keep an eye open for signs of suicidal ideation, like withdrawing from social life, engaging in uncharacteristically reckless behavior (e.g. drug abuse, speeding, unsafe sex), getting their affairs in order (making a will, giving away prized possessions), or outright saying they want to die (even if it’s in a joking manner). The U.S. Department of Health and Human Services estimates that around 60% of people who die of suicide have a mood disorder like MDD, Persistent Depressive Disorder, or Bipolar Disorder. If you need help for yourself or someone else, please contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).



