Alzheimer’s Disease: Everything You Need to Know
Alzheimer’s is not easy, but we’ll help you make sense of its symptoms, treatments, and what it means for your life.






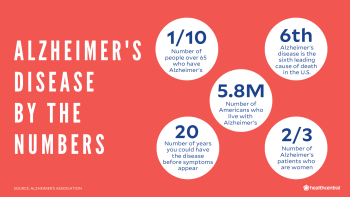
If you or someone you love is having troubling remembering things, you’re probably worried about Alzheimer’s disease, a serious brain condition that gets worse over time. One in 10 people over 65 have it—and scientists think that it may start to develop 20 years before your first symptoms ever appear. While there’s no cure, there are new treatments on the horizon and ways you may be able to slow down the progress. And there is a lot to get a handle on. That's why we talked to top Alzheimer’s experts to give you the knowledge you need on risk factors, treatments, and symptoms so you can continue to live your life. We're sure you have a lot of questions…and we're here to answer them.
What Is Alzheimer’s Anyway?
People talk about Alzheimer’s and dementia as if they are two different things. They’re not. Dementia is used to describe a group of conditions that affect your ability to think, remember, and go about your daily life. It ranges from mild impairment—you have trouble keeping track of the days or balancing a checkbook, say—to a total inability to take care of yourself.
There are many different reasons why you develop dementia, but the most common is Alzheimer’s disease—about 80% of people with dementia have Alzheimer’s, according to the Center's for Disease Control and Prevention (CDC). Mostly, it affects those over 65 (although there’s a rare early onset version that can strike people even in their 30s)—about one in 10 adults over the age of 65 have Alzheimer’s in the U.S., according to the Alzheimer's Association. It’s also a progressive disease, meaning over the span of roughly four to 12 years, it can go from its mild form to its most severe. How fast it progresses tends to depend on the age you first show symptoms: People in their 60s decline faster than those who develop it in their 80s, though researchers don’t fully know why.
To understand Alzheimer’s, it’s good to know how a healthy brain works. Everything we think, do, and feel is the result of billions of nerve cells, called neurons, communicating with one another, sending messages via neurotransmitters to different parts of the brain. To keep the brain cells working, you need just the right amount of blood and nutrients to nourish them and enough glucose (a.k.a. blood sugar) to keep them powered up. When there’s too much debris and too many dead neurons in your brain, immune cells, including the microglia, clean up the mess.
In Alzheimer’s earliest stages—about 20 years before the first signs of the disease show up—the brain’s ability to keep everything running smoothly begins to break down. Here’s a step-by-step of what happens:
A protein known as beta-amyloid begins to build up in the brain. Everybody produces beta-amyloid, but for a variety of reasons—some genetic, some related to aging and inflammation—certain people lack the ability to clear out the excess, which then goes on to form clumps in the brain known as plaques.
Once there are enough plaques in the brain to do damage, another protein called tau, found inside the neurons, also starts to stick together. The tau proteins form long chains that tangle and then extend outside the cells, spreading through the brain, disrupting normal nerve function. And as if these tangles and plaques weren’t enough to deal with, there’s more.
Beta amyloid can also build up in the brain’s blood vessels, making them stiffer and less able to carry blood and nutrients to the cells. That means the brain doesn’t get glucose as efficiently as it once could and it doesn’t process it as well. The result? The brain doesn’t get the energy it needs.
Then, as immune cells try to clear up the plaques, inflammation fires up. Alzheimer’s disease is quite literally the bull inside your brain’s china shop.
This cascade of changes first affects the brain’s temporal lobes and the hippocampus, the parts of the brain involved in forming memory and learning. This is why one of the earliest signs of Alzheimer’s tends to be memory loss (but a particular kind—more on that later). Later more parts of the brain are impacted and more neurons die off, causing the brain to shrink in size. As that happens, people lose more critical thinking skills—like being able to remember events from their childhood or follow a TV show—and they struggle with day-to-day functions like the ability to dress themselves or even control their bladder.
Is There a Cure for Alzheimer’s Disease?
There’s no cure for Alzheimer’s. At its most severe, you lose the skills you were born with, like swallowing, coughing, and breathing. People who die of Alzheimer’s usually die because they stop eating or have impaired swallowing and develop pneumonia or other infections. Or they may die because they can’t take the meds they need to manage another condition, like heart disease or diabetes. Right now, Alzheimer’s is the sixth leading cause of death in the U.S. (at least pre-2020).
It all sounds grim, but there are breakthroughs on the horizon, including a new blood test that can diagnose Alzheimer’s earlier and new medications in clinical trials that can slow the disease down. And because researchers have learned so much in the past decade, even if you’ve been diagnosed with the disease (or know someone who has) there are steps you can take today that can buy you more quality time.
What Causes Alzheimer’s in the First Place?
There are many factors that trigger the build-up of beta-amyloid, although researchers are still trying to understand the particular combination of factors that causes one person to develop full-blown Alzheimer’s, another to have mild cognitive impairment (a precursor to dementia), and yet another to have beta-amyloid plaques but no issues with memory loss (and yes, that can happen—in fact, 40% of people over 90 have already experienced these changes in their brain, but not all these 90-year-olds have dementia). Here is the latest thinking on what exactly contributes to the development of Alzheimer’s:
Age
Alzheimer’s (and other dementias) aren’t a part of normal aging, yet the older you are, the more at risk of developing the disease. But why is the million-dollar question.
It could be that the older you are, the more risk factors you’ve accumulated over the years, like poor-quality sleep, low-grade inflammation, higher blood pressure. Or it could be that the brain changes of age—less volume, fewer new brain cells and lower levels of neurotransmitters—can also set the stage. But whatever the reason, age is the biggest risk factor in roughly 90% of Alzheimer’s cases. And the percentage of people living with Alzheimer’s rises with age: From 3% of those 65 to 74 to 32% of those over 85.
Genetics
Researchers have ID’d more than 40 genes that up your risk of developing Alzheimer’s. One rare mutation, that affects about 1% of people with Alzheimer’s worldwide, runs in families and responsible for the early onset type of disease that strikes when people are in the 30s and 40s.
Another is the APOE4 gene, which plays a role in forming beta-amyloid clumps. One in four people has the APOE4: If you have one copy, you triple your risk for developing Alzheimer’s; if you inherited two copies (from your mom and dad), you increase your risk 12-fold. Then there are genes that can change the way the immune cells like microglia interact with beta-amyloid deposits. Biology isn’t destiny, though—and that’s where other health factors come in.
Your Health
Experts think such chronic conditions that affect your metabolic health (like type 2 diabetes) and blood vessel health (like high blood pressure) may be even more important than genetics for upping the chances of developing Alzheimer’s. Having diabetes or even prediabetes in your 40s and 50s can increase inflammation in the brain and raise your blood sugar levels, all of which makes it easier for beta-amyloid to form clumps.
High blood pressure can damage the small blood vessels in the brain and choke off blood flow, causing dead tissue called lesions. High cholesterol and fats in the blood can also cause inflammation, making it more difficult for the cells to clear up the proteins.
Your Gender and Race/Ethnicity
About two-thirds of all Alzheimer’s patients are women, according to the Alzheimer’s Association 2020 report. Experts used to attribute the difference to female longevity—women lived longer than men, so were more apt to develop dementia in old age. But one study speculated that menopause, and the hormonal shifts it brings, might account for the important changes in the brain like producing more beta-amyloid that contribute to Alzheimer’s.
Blacks and Latinos also develop Alzheimer’s at higher rates—African-Americans are twice as likely to develop the condition (along with other dementias) and Latinos are 1.5 times more likely. This may have something to do with their higher rates of other diseases like diabetes and high blood pressure.
Poor Sleep
Not sleeping well—waking up frequently, difficulties nodding off—was associated with a higher level of risk, especially if you have the APOE4 gene, one study found. One reason why too little shut-eye can lead to the increased risk: Researchers from Boston discovered deep sleep (the type most often interrupted when you don’t get enough z’s) enables the fluid in your brain and spinal cord (the cerebrospinal fluid) to clear out the debris in your brain.
Obesity
Being overweight in your 40s and 50s may play a role in Alzheimer’s, as it also ups your chances of having diabetes, poor heart health, and chronic inflammation—all important risk factors. But you don’t want to lose too much weight as you age. Having a slightly higher-than-average body weight in your 70s and 80s seems to be a protective factor. The reason? It may be a sign your brain is getting enough energy whereas being too thin may mean your brain is starving.
Alcohol Use (and Abuse)
It’s better to have one drink a day than to binge drink or abstain completely, according to one study of roughly 3,000 people aged 72 years and older. Moderate drinking (defined as fewer than 14 drinks a week) may lower the risk of dementia.
The caveat: Moderate drinking may not be as good for you when you have trouble remembering appointments and paying bills, a condition known as mild cognitive impairment (MCI). People with MCI who continued to indulge in their once-a-day habit or, worse, drink more than 14 drinks a week, were at greater risk for developing dementia, including Alzheimer’s.
Depression
Experts don’t exactly know what the link is between depression and Alzheimer’s (as well as other dementias). Being chronically depressed throughout your life can make you more prone to developing Alzheimer’s, studies suggest. This may have something to do with elevated stress hormones that negatively affect your hippocampus (the part of the brain that plays a role in memory). But having depression in later in life could also be one of the earliest signs of Alzheimer’s. British researchers found that people over 50 with depression were 65% more likely to develop the disease.
What Are the Signs of Alzheimer’s?
First off, everyone has trouble remembering things, especially as they get older. The name of the nice mom who lives down the street might slip from your mind when you run into her at the supermarket, for instance, or you might grapple to remember that great Italian place you’ve been dying to try.
The best analogy we’ve heard between normal memory loss and the loss that happens with Alzheimer’s comes from one of our pro panelists, Dr. Andrew Budson, a professor of neurology at Boston University and the co-author of Seven Steps to Managing Your Memory. So we’re going to share it with you just as he explained it to us:
Think of your memory like a filing system, complete with a clerk—your frontal lobes—and a filing cabinet—your hippocampus. The frontal-lobe file clerk brings in information from the outside world and puts it into the memory file. In normal aging, the frontal lobe file clerk may be a little slower, so it takes her longer to retrieve the memory. Or she may not hear as well, so the info needs to be repeated a couple of times before she gets it. Or she may not see as well, so she needs a cue. All of this is normal. The memory is there, it just may take a while and a few hints before you can dredge it up.
In Alzheimer’s, it’s as if the filing cabinet has a huge hole that’s swallowed the information. The filing clerk may be super-efficient, but once the info gets into the cabinet, it disappears and you cannot retrieve it, no matter how many clues you get.
In its mild form, this means that recent memories start to vanish but you can still do everyday tasks without much help, including drive or possibly even work, as long as your job isn’t that complicated. As the disease progresses into dementia, even activities you enjoyed become nearly impossible. Usually, you (or family members) can see changes happening over six-month periods and certainly year to year. Here’s what this looks like:
Memory issues:
You repeat stories or ask the same questions over and over again,.
You spend hours searching for your wallet or cell phone or routinely lose them.
You get lost while traveling a familiar route.
These are often the first signs of the disease. Later, in its moderate phase, you have a tougher time remembering longer-term memories, information you learned a while ago, and recognizing friends and relatives. You get confused more often and may start to wander. At its end stages, you don’t recognize anyone.
Trouble communicating: In its mild form, you often have to search for the right word (which family members fill in for you). Or your conversations have frequent pauses. Later, you have trouble following conversations or even comprehending them.
Difficulties solving problems and doing everyday tasks: You were a gourmet cook who can no longer follow a recipe. Or you were the tech whiz who’s stumped by the smart TV. As the disease gets worse, you struggle with the simplest things, like making a sandwich or dressing yourself. You become incontinent and really need someone around to help with the basics.
Changes in behavior and mood: While people in the mild stage may become depressed or irritable, most personality changes occur in the moderate stage. That may be because the disease has spread to the parts of the brain that control emotion (like the amygdala). And the confusion you feel may be fueling these changes too. So, for instance, you can have outbursts and lash out, become paranoid or at least suspicious of others, or become apathetic. Your circadian rhythm might be off too, meaning you’ll sleep more during the day and be up more at night, or not sleep well at night at all.
When Should I See a Doctor?
Honestly, as soon as you (or your partner or family member) notice you’re having issues remembering important stuff or have issues making decisions or solving problems, head to your provider. You may not have Alzheimer’s or any other form of dementia at all, and instead have a medical condition—low thyroid or low levels of vitamin B12—that’s causing your brain fog. So a checkup can rule that out.
But even if you are experiencing mild cognitive impairment or even mild Alzheimer’s, getting help now may be enough to keep you at this stage instead of slipping into the more serious forms of the disease. A doctor can recommend drugs and lifestyle changes that can keep your memory stable for a couple more years, and even longer. It’s never too late though. Medications exist that can help people in the throes of dementia function better and retain more of their personality.
Unfortunately, too many people don’t get the help they need. Fewer than half of people over 45 who notice they’re having memory issues (called subjective cognitive decline) discuss their worries with their providers, according to the Centers for Disease Control and Prevention. And even though Medicare requires providers to test your thinking skills at your wellness exams if you are 65 or older, about 47% of doctors don’t, according to the Alzheimer’s Association—either because they don’t have the time to do one or their patients aren’t showing symptoms.
Your primary care provider should be able to do a brain scan, some cognitive testing, and rule out underlying conditions. But if your doctor doesn’t have the time or tells you it’s all part of normal aging, then by all means see if you can find a neuropsychologist, a cognitive behavioral neurologist, or a neuropsychiatrist or geriatric psychiatrist.
How Do Doctors Diagnose Alzheimer’s?
First off, there are many conditions that can affect your thinking, so you’ll have to go through a series of diagnostic tests to see if you have some other condition that can explain these memory issues. It’s a good idea to take along someone close to you who can also answer a doctor’s questions and weigh in on what’s been going on.
There is a blood test in the works that will be able to screen for Alzheimer’s even before symptoms appear. The blood test can detect the beta-amyloid and tau proteins and distinguish between Alzheimer’s and other dementias, something that is harder to do now. It’s still a few years from becoming standard, but it’s exciting news and promises to be a game-changer in terms of diagnosis and treatment.
For now, doctors rely mostly on these tests to make a diagnosis:
Physical exam and complete medical history: Your provider will want to hear about your family history (maybe one of your parents had Alzheimer’s or another form of dementia) as well as how your memory and thinking has changed over the past several years. Bring a list of the medications you take now and certainly bring up any chronic conditions you may have (especially if you are seeing a new provider).
Blood and urine tests: Your provider is looking for clues to see if you have a thyroid condition, low levels of vitamins (like B12), Lyme disease, or a chronic UTI that might be triggering these changes.
Cognitive exams: Your memory, problem-solving, focus, and language skills will be put to the test with a 10-minute pencil-and-paper exam. You’re scored according to correct answers for a total of 30 points and anything lower than 26 is considered a sign of cognitive impairment. Tests include:
Mini Mental State Examination (MMSE): You’ll be asked, among other things, to count backwards from 100 by 7s (or spell a word backwards); to recall dates and which city you live in; to draw shapes, follow instructions, and remember words.
Montreal Cognitive Assessment (MOCA): This test is similar to the MMSE, but also asks you to draw a clock when the time is 11:10, connect letters with numbers, and identify pictures of animals. You also have to remember words in a certain order (and no, they’re not person, man, woman, camera, TV) at the beginning of the test and at the end.
Cerebrospinal fluid (CSF) analysis: A doctor will insert a needle in your spine to collect the fluid and check for beta-amyloid and tau proteins. This isn’t usually part of a standard evaluation—most people are freaked out by this—and it’s not always covered by insurance, so doctors will do a lumbar puncture only if they aren’t sure whether you have Alzheimer’s or another type of dementia.
Imaging tests: Doctors will give you a CT scan or MRI to rule out any surprises—a stroke, brain tumor, or fluid accumulating in the brain. Either test can show doctors if you have lesions (dead tissue) or signs of tiny strokes. But doctors prefer MRIs as they give a more detailed picture of the structure of the brain.
If a doctor isn’t positive you have Alzheimer’s (which happens about 10 to 15% of the time) after all these tests, there are other types of imaging tests that aren’t included in standard evaluation.
Flurodeoxyglucose positron emission tomography (FDG PET) helps doctors see how your brain is working. A radioactive tracer containing sugar is injected into your vein via an IV. Then doctors measure the way your brain metabolizes glucose (which it needs for energy). Different types of dementia have different patterns of activity (usually lower) in different parts of the brain. In Alzheimer’s, for instance, there’s lower activity in the middle part of the brain (the temporal and parietal lobes) instead of, say, the front or the back (like other types of dementia). These tests are good for people who already have dementia and Medicare and some other types of health insurance often cover it.
Amyloid PET scans use a radioactive tracer that sticks to amyloid plaques so they show up on the scan. Providers typically will use an amyloid PET scan on patients younger than 70 who have memory loss to determine whether they have Alzheimer’s or something else, as the scan can detect changes early. But even though they’re FDA-approved, no insurance (not even Medicare) will pay for them unless you are part of clinical trial or research. So expect to pay around $3,000 and as much as $5,000 out of pocket.
Tau PET scans are only used for research and aren’t available to most doctors yet, even though they’ve been approved by the FDA. These tests use a radioactive tracer that attaches to the tau tangles.
What Are the Best Alzheimer’s Treatments?
There’s no cure for Alzheimer’s. And there’s no drug that can stop the actual progress of the disease, either, at least not yet. That could be changing in the next few years, but for now, there are only two types of drugs that are approved to treat the disease itself. Both types act on certain neurotransmitters in the brain.
Cholinesterase Inhibitors
These three drugs stop the breakdown of acetylcholine, one of the neurotransmitters most affected by Alzheimer’s in the beginning. Acetylcholine plays a big role in memory formation as well as sleep regulation.
Boosting acetylcholine levels can restore memory and other cognitive skills like judgment, language, and problem solving, to the way they were six months or even a year before, if you have mild Alzheimer’s. The effects can last for a couple of years in some people, but some people may just see moderate results temporarily. And it will only reset your memory, not stop it from deteriorating.
If you’re in the moderate stage, these drugs may not help your memory, but they can help with behavior (such as outbursts or confusion) and function (such as being able to do more tasks). Side effects for all these include nausea, vomiting, and loss of appetite. They are:
Aricept (donepezil)—used to treat confusion for all stages of Alzheimer’s disease, comes in tablet form
Razadyne (galantamine)—used to improve memory and awareness, approved for mild-to-moderate stages, comes in tablet form
Exelon (rivastigmine)—used to treat dementia in mild-to-moderate Alzheimer’s, comes in a capsule or patch
Namenda (memantine)
This drug blocks glutamate and is for people with moderate-to-severe Alzheimer’s, which as it worsens and spreads through the brain affects more neurotransmitters. Glutamate is another neurotransmitter that plays a role in learning and memory. Alzheimer’s patients produce more glutamate than normal—and while that may seem like a good thing, it isn’t. Too much glutamate in the brain overstimulates neurons and damages them, causing them to die off.
Namenda, which comes in a liquid or capsule, can help improve attention, alertness, mood, and behavior and can give people a few more months of independence as they go about their self-care and simple tasks. It may help clear confusion and drowsiness, but it can also cause more.
Namzaric (memantine + donepezil)
If you're already taking Aricept or another cholinesterase inhibitor, but need the extra boost to function better, this drug combines the two to temporarily slow down symptoms and improve thinking. The side effects include dizziness, headaches, nausea, and vomiting.
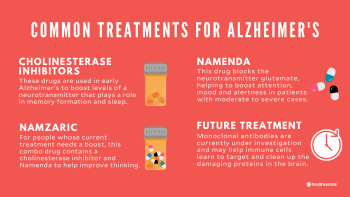
Future Treatments Currently Being Studied
The medications that are available right now can’t stop the disease or prevent it. But that could be changing, as researchers work on immunotherapy drugs that harness your immune system to fight the disease, medications that can reduce inflammation or the way the microglia reacts with beta-amyloid, and even vaccines that you can take in your 40s to prevent beta-amyloid from clumping together in the first place.
Monoclonal antibodies are among the most promising. These types of drugs use antibodies to target the proteins doing the damage in your brain in the hopes that they’ll stimulate the brain’s immune cells to clear them up. There are several in clinical trials now, but the closest drug to being approved is aducanumab, which targets beta-amyloid and injects the antibodies via an IV infusion once a month. The results of various studies have been mixed, but high doses of aducanumab seem to work best in people in the disease’s early stages, so that the microglia can chew through the clumps before they do more damage. The FDA will decide whether to approve the drug in 2021.
Treatments for Individual Symptoms
People with moderate Alzheimer’s and other dementias can suffer from a host of other symptoms, ranging from depression and anxiety to sleep issues and aggressiveness. But because many of the meds used to treat these symptoms can cause more problems, doctors try to avoid them unless the issue is so severe that all sorts of behavior-modifying tactics (like distraction, soothers and avoiding triggers, taking walks or drives) aren’t working any more. These drugs include:
Anti-anxiety drugs—to treat agitation. These should be used sparingly as they can cause dizziness, sleepiness and up the chances of a fall. Drugs include Xanax (alprazolam), Ativan (lorazepam), and Valium (diazepam).
Anti-depressants—for irritability, general anxiety, or depression. These are generally safe to take but talk to your doctor. Medications include Prozac (fluoxetine), Zoloft (sertraline), and Celexa (citalopram).
Anti-psychotics—for extreme aggression, hallucinations, and delusions. This type of med can increase the risk of stroke in older folks with dementia, so it’s a medication of last resort. Drugs include Abilify (aripiprazole) and Seroquel (quetiapine).
Can I Take Steps to Prevent or Minimize Alzheimer's?
Yes you can—and it’s by doing many of the same things you do to keep heart disease at bay. Experts now think that what’s good for your heart is good for your brain. Even if you are experiencing the first signs of memory loss and cognitive decline, you may be able to stave off the worst effects by eating right and exercising as well as taking medications to manage any chronic conditions you have. People may already be getting the message. Researchers have found that the rates of dementia among people of European descent in the U.S. are actually going down—in the last 30 years they’ve declined 13% per decade.
Here’s what seems to help:
Exercise: For now, physical activity is the closest anyone’s come to preventing Alzheimer’s or at least keeping it at bay for a few more years. Try for a brisk 20 minute walk or run a day (or break it up into 10 manageable-minute chunks), and you’ll be stimulating your brain to produce more neurons, especially in the hippocampus. You’ll also reduce your risk of strokes, sleep better, and improve your mood (especially if you walk on a nature trail), all of which contribute to keeping your brain (and body) healthy.
Even if you have Alzheimer’s, exercise can help improve your memory and thinking skills as well as your boost mood and quality of life. Along with doing something aerobic, work in some yoga or strength training to keep muscles and bones strong so falls are less likely (or damaging).
A healthy diet: For most people, a Mediterranean-style diet—heavy on produce, legumes, lean meat and fish and less reliant on simple carbs, processed or fatty meats, and sugar—can reduce inflammation in the body and brain. And it can keep you from developing type 2 diabetes and other metabolic conditions that can up your risk.
Kicking bad habits: If you smoke quit. If you’re downing more than two drinks a day—or you save your booze consumption for a weekly splurge of several margaritas in a sitting—you’ll need to cut back (and rethink). While researchers still think that alcohol may protect the brain, moderation is key. Too much alcohol, especially if you are already showing symptoms, can tip you over into dementia.
Taking your meds: If you have high cholesterol or blood pressure, now is the time to manage these conditions. Besides diet and exercise, talk to your provider about medications that can lower both so you protect your heart and brain.
Keep your brain working and engaged: We’re not talking about brain games (though if you love puzzles, keep doing them). But picking up new skills (learning to knit or auditing a college class) as well as seeing good friends, joining a club or support group, or volunteering can lower your risk for Alzheimer’s too.
Staying safe: The brain is especially fragile at the earliest stages of Alzheimer’s, and any type of major event like a fall, a mini stroke, or a serious illness can accelerate the progress of the disease.

What’s Life Like With Alzheimer’s?
Getting a diagnosis is a blow, and we’re not going to lie, it’s almost impossible not to feel anxious or depressed. Doctors already know more than they did even 10 ago and have found evidence-backed ways to buy you more quality time—by adopting healthier habits, simplifying your routine, and taking the memory-boosting medications already on the market.
That said, Alzheimer’s can be a serious and sad disease for those who have it. As it slowly progresses, it will rob you of your independence. At first, you’ll just need someone to help you pay the bills on time, do errands, and even drive. Later on, you’ll need a caregiver that can help you make food, bathe you, and dress you.
It’s also hard on your loved ones. The cost to families through out-of-pocket care expenses is huge—and family caregivers (mostly women) who cut back their hours or take time off to care for their parents or partners take a financial hit too. That’s why it’s crucial to find support from people going through what you are, whether you have Alzheimer’s or care for someone who does.
There is hope though. One day in the not-so-distant future Alzheimer’s will become a disease you can live with and manage, sort of the way many people with cancer do now. Already there are clinical trials underway for new medications, as well as studies involving thousands of Americans that measure the impact of lifestyle interventions on memory and thinking. While none of these treatments may prevent or cure the disease, they may be able to give you 10 or 15 years without its debilitating symptoms, and more time to enjoy a happy and productive life.
Where Can I Find Alzheimer’s Disease Communities?
If you’re looking for a support system, it’s likely that you or someone very dear to you has been diagnosed with Alzheimer’s disease. Or maybe you’re just in the “suspecting” stage and want to gauge how others have navigated this very confusing and overwhelming time. There’s no one who can quite understand it and guide you like the caregivers who have been there—and those who are still in it, every day. If you’re new to this world, these are the people and organizations to follow and join ranks with, so that you never quite feel alone.
Top Alzheimer’s Disease Caregivers and Support Groups on Instagram
Nikki DeLoach, @nikdeloach
Follow because: She wears many hats, but one of her post prominent and passionate is that of spokesperson for the Alzheimer’s Association. She comes from a long line of family members with Alzheimer’s or related diseases, and she shares the hardships of caregiving along with plenty of encouragement to keep going and keep loving on her feed.
Alzheimer’s Caregiver Support, @alzheimerscaregiversupport
Follow because: Their inspirational quotes and encouraging stories will be become like a daily mantra, reminding you every day that you can do this.
Alzheimer’s Support, @alzheimerssp
Follow because: They often highlight families who are going through exactly what you are, and when you click through to their profile you can see that they live very normal, albeit sometimes challenging, lives, but they get through it all — together.
Carol Bradley Bursack, @mindingourelders
Follow because: Every single post is a question from someone like you—someone trying to navigate early stages, next steps, finances, housing, and everything in between in this unknown new world. Carol answers every question as a longtime caregiver, and someone whose own story began decades ago when she cared for her father with dementia.
Top Alzheimer’s Disease-related Podcasts
The Forgetting. What’s so very unique and enticing about this podcast is that it’s hosted by two friends—one who has Alzheimer’s disease, and one who doesn’t. Greg O’Brien, who was diagnosed with early-onset Alzheimer’s in 2009 talks with friends and author, David Shenk about his evolving symptoms and what goes on in his mind.
Mind What Matters. Hosted by Nikki DeLoach, spokesperson for the Alzheimer’s Association, this podcast not only dives deep into conversations with experts like neurologists and speech therapists, but also with caregivers who are making daily tough decisions on the best care and next steps for their loved ones.
Alz in the Fam. They are just one of the 16 million families caregiving for someone with Alzheimer’s disease, and they are sharing every step of their journey, from their mom’s diagnosis, to hiring a caregiver, to working through the process with siblings, and more.
Alzheimer’s Speaks Radio. It’s not just sound bites about living with Alzheimer’s, it’s in-depth stories and experiences from those living with, caring for, and treating the disease. Join host Lori La Bey as she talks to people all over the world, from all walks of life, who are directly affected by Alzheimer’s disease.
Where Can I Find Support?
These groups can put you in touch with support groups, clinical trials, research and events where you can volunteer.
Alzheimer’s Association. This group has been around since 1980 and takes a lead in funding research and holding scientific forums and events. You can find your local chapter, which can put you in touch with support groups, social activities for patients and caregivers, and education and training sessions. It also offers a TrialMatch program, where you can participate in a clinical trial or research study, whether you have Alzheimer’s (any stage), are a caregiver, or just a healthy person interested in volunteering.
Alzheimer’s.net. An online community, this site can help you find care for Alzheimer’s or dementia patients in your state, as well including clinical trials and dedicated research centers where you can find information, doctors, and support groups.
Alzheimer’s Foundation of America. Call the toll-free number for this educational and advocacy nonprofit and you’ll be connected to a social worker who can give you information and put you in touch with services to make your life easier. The organization also offers educational webinars as well as virtual art therapy classes.
Alzheimer’s Xplained USA. A team of doctors and artists banded together to form this Facebook group that can answer your questions about your diagnosis and other medical information. The group has about 8,500 members.
Alzheimer’s and Dementia Caregivers Support. With nearly 53,000 members and 150 posts per day you are sure to find people weighing in on a topic or struggle that’s consuming you right now—without anyone getting judgy about it.
Alzheimer’s is a type of dementia and the most common one. About 80% of people with dementia have Alzheimer’s disease, and about 1 in 10 adults over 65 have Alzheimer’s.
Having a first-degree relative who had Alzheimer’s can up your chances of getting it by around 10% to 15%. But it’s important to remember that you can actually decrease your risk by nearly a third by following the steps to stay heart-healthy. What’s the connection? Conditions like high blood pressure and diabetes up your risk of Alzheimer’s, too.
Experts think that exercise, a healthy diet, a rich social life (volunteering, say, or book clubs), quitting smoking and avoiding binge drinking can be just as important for your brain as it is for your body.
Not yet. At best the medications for the disease can set back the clock, but they can’t stop the disease’s progress. But that may be changing. There is a new blood test in the works that can spot Alzheimer’s early on, when lifestyle changes can minimize the memory loss. And there are new drugs being tested that may slow the progress of the disease so people can work, drive, and continue with their lives for longer.
More Like This
New Research About What Causes Alzheimer’s in Women
Medically Reviewed
Do You Know the Warning Signs of Alzheimer’s Disease?
Medically Reviewed
Is the Only FDA-Approved Treatment for Alzheimer’s Worth the Hype?
Medically Reviewed
Does Benadryl Cause Dementia?
Medically Reviewed
More Stories You Might Like...
Is Estrogen Loss Behind Women’s Nearly Doubled Risk for Alzheimer’s Disease?
Medically Reviewed
When Dementia Comes on Fast
Medically Reviewed
You Are Not Alone: Caregivers Share Their Experiences
