Multiple Myeloma: Everything You Need to Know
We've got the doctor-approved scoop on multiple myeloma causes, symptoms, treatments, and a jillion other facts and tips that can make life with MM easier.






Whether you’ve just been diagnosed or worry you could have multiple myeloma, you’re probably nervous, confused, and maybe even a little scared. That’s normal, and everyone featured on HealthCentral with a chronic illness felt just like you do now. But we—and they—are here for you. On this page alone, you’ll discover the realities and challenges of the condition, but also the best treatments, helpful lifestyle changes, where to find your multiple myeloma community, and all the crucial information to help you not merely manage—but thrive. We’re sure you’ve got a lot of questions...and we’re here to answer them.
What Is Multiple Myeloma, Exactly?
Everyone has heard of breast cancer, lung cancer, even colon cancer. But when you say, “multiple myeloma,” you might get a lot of blank looks. Multiple myeloma (MM) is fairly rare—it’s a blood cancer that starts in the bone marrow, and it happens when certain white blood cells known as plasma cells mutate and grow out of control.
People with multiple myeloma develop tumors in their bone marrow, sometimes in more than one spot. As these tumors take up more and more space inside the bones, they keep healthy bone marrow from doing its job of making infection-fighting white blood cells and red blood cells, which carry oxygen around the body.
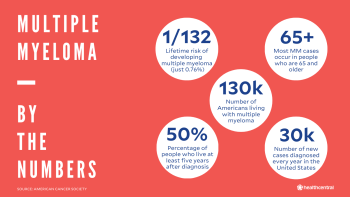
The average American’s risk of getting MM (also known as Kahler disease or plasma cell myeloma) at some point in their lifetime is just one in 132. (Compare that with the number of women who will develop breast cancer, which is one in 12.) About 30,000 cases of MM are diagnosed every year, and there are an estimated 130,000 people living with it in the U.S. today.
Like any cancer, MM is a serious condition. But people with the disease have a much brighter future today than they did even 10 years ago. Several new treatments have been approved in the last decade, and survival rates keep going up.
Today the percentage of people who live at least five years after diagnosis is over 50%. For people who are diagnosed at early stages of MM, the outlook is even better—the 5-year survival rate is over 70%.
Multiple Myeloma Stages
MM is broken up into four basic categories, or stages, that are used to describe how much the cancer has spread and help your medical team decide on the best treatments.
Pre-Cancer Stage: “Smoldering” Multiple Myeloma
Despite its dramatic name, smoldering multiple myeloma (SMM) isn’t cancer yet—it’s a precancerous condition that can become full blown myeloma. But for reasons still not entirely understood, most people diagnosed with SMM don’t go on to get cancer.
There’s a 10% chance of progression for the first five years after being diagnosed with SMM; the risk then falls to 3% for the next five years. Ten years after diagnosis with SMM, the chances that it’ll become cancerous is just 1% per year. Most people with SMM don’t need treatment, but they will be monitored closely.
Usually, there are no symptoms of cancer in someone with SMM, and the diagnosis only occurs because doctors spot abnormal readings during a blood test for something unrelated. With better research, doctors are learning how to determine which cases of SMM have the highest risk of progressing to cancer. In fact, a 2020 study by researchers at the Dana-Farber Cancer Center in Boston, MA, identified RNA changes in certain immune system cells that suggest an increased likelihood of a person developing multiple myeloma. Studies are also being done to figure out if treating SMM with anti-cancer medications can help halt the progression.
Stages I, II, and III
Staging of multiple myeloma depends on how many cancer cells there are, how many tumors or areas of damage there are in the bones, and what your blood levels are for calcium, hemoglobin, and a substance called monoclonal immunoglobulin.
In the earliest stage of multiple myeloma, Stage I, only a small number of cancer cells are found. Bone x-rays show just one area of damage, or none at all, and the other measures are normal or just slightly off.
In the most advanced stage, Stage III, there are large numbers of cancer cells, three or more spots of bone damage, and at least one of the other tests (hemoglobin, blood calcium, or monoclonal immunoglobulin) are concerning. Any cancer that lands somewhere in the middle is considered Stage II.
What Causes Multiple Myeloma?
Doctors don’t know exactly what it is that triggers blood plasma cells to grow out of control, but we do know a few key things that contribute to the likelihood. One has to do with our DNA. DNA contains genes that tell the cells in our body how to behave.
“Oncogenes” trigger cell growth, while “tumor suppressor genes” slow it down. When there are mistakes and mutations in a person’s DNA, it can turn these genes on or off, potentially leading to multiple myeloma. Research suggests that the most likely cause for MM is random mutations in these genes that happen during a person’s lifetime.
Another component of our DNA, called chromosomes, may also play a role. Normal human cells have 46 chromosomes. But MM cells are often found to be either missing a part of one chromosome or have chromosomes that are mixed up and switched out of their proper order.
These are other risk factors associated with MM:
Family history. Most people with MM don’t have a family history of the disease. That said, if you do have a parent or sibling who has MM, you are at a slightly higher risk for it than someone without close relatives with myeloma.
Age. Simply getting older increases the risk of developing MM. Most cases happen in people 65 years or older; fewer than 1 percent of cases are in people under 35.
Gender. Men are more likely to get MM than women. The reasons why aren’t well understood, but there is likely a genetic factor.
Race. MM is more than twice as common in African Americans as it is in white Americans.
Body mass index. Having a BMI in the “overweight” or “obese” category is linked with an increased risk of multiple myeloma. Emerging research suggests that fat cells within the bone marrow may encourage the growth of MM cancer cells.
Symptoms of Multiple Myeloma
There are usually no signs in the early stages of multiple myeloma. As the disease develops, classic symptoms are often referred to with the acronym CRAB, which stands for calcium, renal, anemia, and bone problems. More on these and other MM symptoms, including:
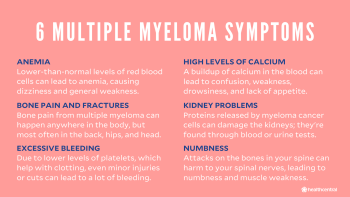
Anemia. Lower than normal levels of red blood cells can lead to anemia, which often causes dizziness, shortness of breath, and a general feeling of weakness.
Bone pain and fractures. Some people with multiple myeloma have bone pain—it can happen anywhere in the body, but most often in the back, hips, and even your head. MM can also weaken bones enough to cause breaks or fractures from minor stress or injury.
Excessive bleeding. MM causes lower-than-normal levels of blood platelets. When that happens, you may bleed a lot even from minor injuries and scrapes.
High blood levels of calcium. Multiple myeloma can lead to a build-up of calcium in the blood. This can lead to confusion, weakness, drowsiness, lack of appetite, stomach pain and constipation, dehydration and severe thirst. Really high levels of calcium can lead to a coma.
Infections. MM slashes the number of white blood cells in your body, leading to “leukopenia,” which can reduce your ability to fight off infections like pneumonia. When someone with MM does get an infection, it can take much longer for treatments to work and they may stay sick for longer than normal.
Kidney problems. Proteins released by myeloma cancer cells can hurt the kidneys. This may show up on blood tests or urine tests.
Numbness. If bones in the spine are attacked by MM, they can start to press down on spinal nerves and lead to numbness and muscle weakness (usually in the legs), or severe back pain that hits quite suddenly. This is a medical emergency and needs immediate treatment.
Pins and needles. Toxins released by cancer cells in MM can damage nerves, leading to a tingling sensation in different parts of your body.
Stroke symptoms. Sometimes, MM can lead to slurred speech and weakness on one side of the body. This is because of slower blood flow to the brain, thanks to proteins released by the cancer cells. If this happens, call your doctor right away to rule out a stroke and do further testing.
How Do Doctors Diagnose Multiple Myeloma?
Doctors use a few different tools to determine if you have MM, including a physical exam and a deep-dive into your symptoms. After that, there are several different tests that can be done, including blood tests and imaging.
Blood and Urine Tests
Myeloma cancer cells pump out an antibody called monoclonal immunoglobulin, or “M protein,” that can be measured in blood and pee. (Once diagnosed, these tests can also be done to figure out if the disease is spreading or treatment is working.)
A doctor may also want to have your blood or urine samples tested for other proteins that can be potential markers of MM, such as immunoglobulin, serum albumin, beta-2 microglobulin, and proteins known as “free light chains.”
Imaging
Experts don’t yet know which type of imaging is the best for diagnosing multiple myeloma—they all have pros and cons—so your doctor may want to employ a couple different tests to cover all the bases. These are a few of the common options:
X-ray. X-rays looking for bone damage are often the first step in imaging, since they’re relatively inexpensive and easy to get.
CT (computed tomography) scan. These computer-aided x-rays can show soft tissues and organs, not just bones, and create a 3D image of the inside of your body. (The injection of dye, sometimes used to create a more-detailed picture, is not used during a CT scan for multiple myelom, because it can lead to kidney damage.)
PET (positron emission tomography) scan. Like CT scans, PET scans take pictures of your organs and tissues. By injecting a very small amount of a radioactive liquid into your blood, your doctor can see how much “activity” is going on in the concerning areas of the body. Active cancer cells suck up this substance more than other cells around them.
MRI (magnetic resonance imaging). MRIs use radio waves and a magnetic field and computer to make 3D images. These scans capture the bone marrow itself, so a doctor can assess how much of the normal, healthy marrow has been replaced by cancer cells. These tests can also pinpoint tumor size and nerve compression.
Other Tests
If blood tests and imaging suggests something’s up, your doctor may move on to other tests to confirm an MM diagnosis, figure out the disease stage, and decide on a course of treatment.
Bone marrow tests. Bone marrow is made up of liquids and solids. Bone marrow aspiration tests the liquid, and biopsy tests the solid. Both tests are done with a needle inserted into the bone, often the pelvic bone, and they’re often done at the same time.
Molecular testing. Detailed genetic testing of the myeloma cancer cells will tell doctors how aggressive the tumor is likely to be and can help determine the best treatments.
Best Treatments for Multiple Myeloma
Treatment for multiple myeloma is different than treatment for other cancers such as breast or lung cancer. It can’t be cured, and it’s known for coming back again and again even after you think you’ve knocked it out. So treatment is generally ongoing—somewhat like managing a chronic illness.
Because multiple myeloma is found in your blood, it is sometimes called a "liquid" cancer. The cancer cells do form clumps, or tumors, in the bone marrow as well, but operating to remove tumors from bone is incredibly complex and dangerous. That's why medications and other therapies are used—they target and kill the cancer without cutting into bones.
The best combination of treatments for your MM will depend on the stage and molecular features of the cancer. These are the most frequently used ones.
Chemotherapy
Chemo drugs kill cancer cells. Although some meds are in pill form, chemo is usually delivered through an IV “infusion” or injection. Doses are given in cycles of a few weeks at a time, allowing you to recover from each treatment before having another. Chemo typically lasts anywhere from four to six months.
Targeted Drugs and Immunotherapy
Rather than killing cancer cells directly the way chemotherapy does, targeted drugs and immunotherapy medications zero in on certain proteins and receptors in cancer cells that slow growth or boost a person’s immune system to help it destroy cancer cells.
These drugs have proved promising, and new ones are being discovered and tested regularly. Current targeted and immunotherapy drugs for MM include checkpoint inhibitors, immunomodulatory agents (IMIDs), immunosuppressants, interferons, monoclonal antibodies, proteasome inhibitors, and cellular immunotherapy using T cells. A 2021 study in the New England Journal of Medicine found that new type of chimeric antigen receptor (CAR) T cell therapy improved cancer symptoms in nearly 75% of participants with multiple myeloma, offering much hope for the future.
Corticosteroids
Corticosteroids, such as prednisone and dexamethasone, are commonly prescribed to patients with MM. They reduce inflammation, swelling, and pain, and may also help with chemotherapy side effects like nausea and vomiting.
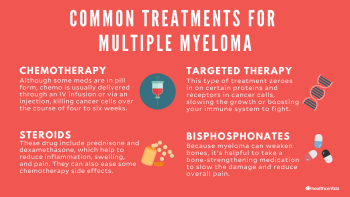
Bisphosphonates
Because myeloma can weaken bones, some people are given these bone-strengthening drugs to help slow down the bone damage and reduce bone pain.
External-Beam Radiation
Radiation treatments use high-energy x-rays to kill cancer cells and help lower the chances of cancer coming back. Treatments are given frequently (sometimes daily) and can last several weeks. Radiation may help with pain and other symptoms of multiple myeloma.
Bone Marrow Transplant
In younger patients and those with an aggressive form of the disease, bone marrow transplants are often coupled with high-dose chemotherapy.
Here’s how it works: Stem cells (called hematopoietic cells) live in the bone marrow and make all of your blood cells. In a bone marrow transplant (a.k.a. stem cell transplant) healthy hematopoietic cells are collected from either you or a donor, and given to you through an IV. They travel to the bone marrow and grow into healthy red and white blood cells and platelets.
When your own cells are transplanted, it’s called an “autologous” transplantation; if the cells come from a donor (usually a sibling), that’s called an “allogeneic” transplantation.
While there is a risk of complications with all MM treatments, bone marrow transplants have some of the highest, including infections and something called graft-versus-host disease (GVHD), in which transplanted stem cells from a donor attack your body tissues, causing inflammation; it’s treatable and rare, but can be life-threatening.
What’s Life Like for People With Multiple Myeloma?
Understandably, being diagnosed with multiple myeloma can turn your life upside down. The future feels scary, treatment can be painful, and you may also have to deal with people who don't understand the condition or what you’re going through.
Here’s the good news: There are more treatments for the disease than ever before, survival rates are increasing at an impressive clip, and more research is being done by the minute into new therapies to keep the cancer at bay and improve people’s quality of life.
Take things one step at a time: Educate yourself about multiple myeloma, never be afraid to ask your medical team questions, and enlist the help of a friend or loved one to go to appointments with you. MM treatment can be complex and the terminology confusing—your appointment buddy can take detailed notes so you can focus on getting better.
You can also help your cause by working stress relief into your daily life. Negative emotions can impact your ability to make thoughtful decisions, as well as lead to hormonal reactions that can suppress your immune system. Incorporate activities that help you quiet your mind such as meditation, deep breathing, exercise, journaling, or any other method that works for you.
And consider attending a support group or talking to a therapist. Being diagnosed with cancer is frightening—even if yours is caught early and you have a sunny prognosis. No one can understand exactly what you’re going through quite like someone who’s experienced it. Many larger hospitals and cancer centers have free support groups for patients. Try one out.
Where Can I Find Multiple Myeloma Communities?
Top Multiple Myeloma Instagrammers/Blogs
Sara Alexis / @iamnottheword
Her style, writing, and photography all capture the vibe of a living life to the fullest with MM. You can feel her connection to nature through her photographs, making her page a relaxing place to land. Even if you just want to enjoy some adorable pictures of seals and penguins, Sara Alexis is the girl to follow.
Donna McNutt / @thecancerfashionista
When McNutt couldn’t get dressed one morning because of severe rib pain, she knew something was wrong. She soon found out she was dealing with MM. Determined to maintain a sense of normalcy during treatment, McNutt dedicated herself to her fashion. Documenting her journey one chic outfit at a time, she drives home the point that multiple myeloma is no match for a woman’s sense of style.
Oscar Chalupsky / @oscarchalupsky
You might recognize Chalupsky as the 12-time world champion Surfski competitor, but these days he’s championing another cause. After he was diagnosed in 2019, he started documenting his journey not only through treatment, but through the rest of his “75% normal” life. If inspiration is your goal, the CrossFit and motivational speech videos on his platform are all you’ll ever need!
Top Multiple Myeloma Podcasts
Medscape InDiscussion: Multiple Myeloma. Joseph Mikhael, M.D., talks to several specialists about innovations in multiple myeloma screening, diagnosis, and therapies. The podcast’s focus on person-centered care leads to conversations surrounding comorbidities and treatments that focus on caring for the whole person. Promoted as offering diverse insights and practical ideas, conversations on this podcast explores powerful innovations in the treatment of MM.
CancerCare: Multiple Myeloma CancerCare Connect Education Workshops. If you’re a science nerd, this is the show for you. CancerCare Connect is an educational program that explains the “why” of different treatments, research methods, and symptoms surrounding MM. This show is great for MM survivors and healthcare professionals alike. While it’s science-based, it’s easy to understand and provides great information on how to interact with your healthcare team while going through treatment.
Living with Multiple Myeloma. Through conversations with both the affected and the caretakers, this podcast explores a full range of topics regarding life with MM. One of the best components of this show is listening to survivors talk about how they went about living a normal life during treatment. These tidbits, intertwined with information about new treatment options, creates the perfect mix of science and real-life experience making listening easy and helpful. Plus, the hosts’ Irish accent makes you feel like you’re in a movie.
Top Multiple Myeloma Non-profits and Support Groups
Multiple Myeloma Research Foundation. There are so many great patient resources provided by the MMRF, including a hotline for the newly diagnosed, treatment guidelines, and mentorship programs. With the hotline operating during normal business hours, this is a great place to go if you have questions and want answers fast. On top of that, nearly 90% of their fundraising efforts go toward research and clinical trials, promoting better treatments, and finding a cure.
International Myeloma Foundation. Quality of life is the main focus of the International Myeloma Foundation, until a cure is found. Led by their four pillars: education, research, advocacy and support, they supply those living with MM and their support systems with all they may need to live a quality life with MM. They have operational teams all over the world, so they’re probably close by.
MyMyelomaTeam. Finding a safe place to talk freely about feelings and worries is beneficial to your mental health while on this journey. My Myeloma Team supplies a social media platform strictly for patients living with MM. You can connect with fellow MM fighters and survivors to get real about treatments, symptoms, remedies, and so much more.
Multiple myeloma (MM) is a type of blood cancer that occurs when certain white blood cells mutate and start growing out of control. People with MM develop tumors in their bone marrow that prevent healthy marrow from doing its job of making infection-fighting white blood cells and oxygen-carrying red blood cells.
Doctors don’t know exactly what causes multiple myeloma, but it likely comes down to DNA damage and chromosomal differences. Normal human cells have 46 chromosomes, but multiple myeloma cancer cells are often found to be either missing a part of one of chromosome, or have a mixed up order of chromosomes.
No, it’s not considered curable—yet. But it is treatable. Many new treatments have been discovered in the last decade, and some doctors are starting to call it a “chronic” condition that can be managed successfully for years.
Yes. Multiple myeloma used to be known as Kahler (or Kahler’s) disease, named after Otto Kahler, the doctor who first discovered it in 1889. Other names for multiple myeloma are myelomatosis and plasma cell myeloma.
More Like This
How to Help Your RRMM Meds Work Better
Medically Reviewed
Should You Try a Clinical Trial for Relapsed Refractory Multiple Myeloma?
Medically Reviewed
Fifth Time’s a Charm for RRMM
Medically Reviewed
What Your Hematologist Wants You to Know About RRMM
Medically Reviewed
More Stories You Might Like...
What to Expect During Relapsed/Refractory Multiple Myeloma Treatment
Medically Reviewed
Expert Tips for Making It Work With Multiple RRMM Meds
Medically Reviewed
How Combination Therapy Works for Multiple Myeloma
Medically Reviewed
Multiple Myeloma Causes
Medically Reviewed
