Rheumatoid Arthritis: Everything You Need to Know
Get the doctor-approved details on rheumatoid arthritis causes, symptoms, treatments, and other facts and tips that can make life with RA easier.






Whether you’ve just been diagnosed or worry you could have rheumatoid arthritis, you’re probably nervous, confused, and maybe even a little scared. That’s normal, and everyone featured on HealthCentral with a chronic illness felt just like you do now. But we—and they—are here for you. On this page alone, you’ll discover the realities and challenges of the condition, but also the best treatments, helpful lifestyle changes, where to find your rheumatoid arthritis (RA) community, and all the crucial information to help you not merely manage—but thrive. We’re sure you’ve got a lot of questions...and we’re here to answer them.
What’s Rheumatoid Arthritis?
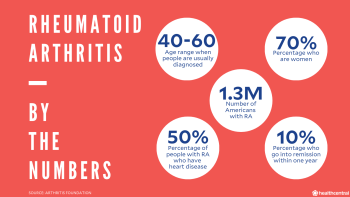
The term “arthritis” feels familiar because: Who hasn’t seen the stock image of elderly-person-gripping-knee? But in fact, the word is often used incorrectly. First, “arthritis” is a catchall term; there isn’t just one variety. Rheumatoid arthritis (RA) is the second most-common type, affecting approximately 1.3 million people in the United States, 70% of whom are women, according to the Arthritis Foundation. Second, RA doesn’t affect only the retirement set, nor does it hit just knees and hands. RA is an autoimmune disorder that causes systemic inflammation, which primarily infiltrates the joints but also has effects beyond them. While it can occur at any time, RA typically develops between ages 40 and 60. That being said, RA can also affect children via a condition called juvenile idiopathic arthritis.
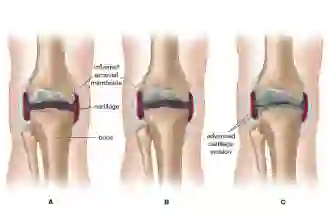
To really understand RA, it helps to have an image in your mind of how joints work. So, picture this: Joints contain several structures that allow you to move easily.
When healthy, the ends of the bones in a joint are protected from rubbing together by an elastic slippery material called cartilage (yep, the same stuff your ear is made of).
The entire joint is surrounded by a capsule, known as the synovial sac.
A thin layer of tissue called the synovial membrane lines the sac.
The membrane secretes lubricating synovial fluid, which reduces friction, protecting the cartilage and joints during movement.
But here’s what happens when RA strikes: The immune system essentially misfires and sets its sights on the synovial membrane, attacking as if it’s a foreign invader.
In the early stages, the synovial membrane becomes inflamed and thickened, causing pain and limiting joint movement. Some people report feeling a warm or even burning sensation around the affected joints as well as a stiffness that makes movement slow. Over time, untreated inflammation can damage cartilage and bones. The space between bones can become smaller, causing joints to become unstable, misaligned, more painful, and sometimes even immobile.
Eventually, inflammatory tissue begins to build up, sometimes causing nodules to form around the area, most commonly along the back of the forearms, elbows, joints, and pressure points such as sacrum, occiput, and heel. These nodules will fluctuate with disease activity. However, if you imagine someone with arthritis in their hands, the very firm nodules at the furthest finger joints are actually those seen in Osteoarthritis and not rheumatoid arthritis. And while RA is known for causing joint pain and inflammation, it can spark other symptoms throughout your body, including dry eyes, chest pain, and osteoporosis.
Worth noting: Before you feel any joint pain, it’s common to experience general, nonspecific RA symptoms; unfortunately, they’re the kind that seem to go with everything–fever, fatigue, loss of appetite—so linking them with RA doesn’t often happen. And that tightness you feel in your joints may only be an issue in the morning (making it seem like not such a big deal). With rest, any synovial fluid you have is soaked up by the cartilage, much like a sponge absorbs water. As you move, the cartilage is “squeezed,” and the fluid bathes the joint. First thing in the a.m., there’s just not going to be a lot of extra fluid to keep things loose. But the more you move, the more fluid is released.
What Causes Rheumatoid Arthritis?
Scientists believe that the overactive immune response that precipitates RA is triggered by a complex interaction between genetic and environmental factors. Ital on the complex part, because not even the top minds in medicine have figured out the exact cause of rheumatoid arthritis. Conditions as diverse as periodontal disease (or gum disease) and Epstein-Barr virus, which causes mononucleosis, have been linked to RA. As scientists continue to chip away at the mystery, a few specific correlations have been identified or are currently being investigated:
Genetics
Certain genes increase the risk for developing rheumatoid arthritis. For example, the genetic marker HLA-DR4 has been found in 60% to 70% percent of people of European ancestry with RA. But, what’s a “genetic marker”? It’s any variation in your DNA that may indicate an increased risk of developing a specific condition. However, simply having the gene does not mean that you have RA or that you will develop it. Because there are so many other factors that impact the development of rheumatoid arthritis and because the gene alone cannot confirm diagnosis or predict it in the future, docs do not perform genetic testing when diagnosing RA.
Being a Woman
Since women get the disease three times more often than men, some experts believe hormonal factors may play a role in causing rheumatoid arthritis. It has been shown that estrogen can rev up the B cells (those are the white blood cells that attack the synovial membrane) and thus exacerbate autoimmune diseases like RA.
Viruses and Infections
While we know that RA occurs because the immune system attacks the body’s healthy tissue, the medical jury’s still out on the cause for that response. Some researchers believe that healthy cells may get mixed up in the action when the body senses danger from a virus or infection; when the immune system kicks into gear and attacks the germs (aka an immune response), the body’s own tissue may get assaulted, too. That's when autoimmune diseases like RA pop up, and healthy joints fall under siege.
Rheumatoid Arthritis in the Hands
RA typically starts in the hands or feet and later spreads to larger joints like knees and ankles, so it’s common to see the first signs of it here. You might notice stiffness, especially in the morning, and joint swelling, tenderness, and warmth.
Treatments for Rheumatoid Arthritis in Hands
There are several ways to treat RA in your hands, from medicine to inexpensive home treatments. Talk with your doctor about oral and topical anti-inflammatory medications that may help and surgical options. You may also want to change your diet or purchase some inexpensive items that could help, such as arthritis gloves.
Osteoarthritis vs Rheumatoid Arthritis in Hands
Osteoarthritis in hands is the most common form of the condition, caused when cartilage in the joints starts to break down and cause pain, stiffness, and inflammation. It primarily affects older people, while RA is most common in people ages 30 to 50. RA in the hands also causes pain, stiffness, and swelling but will come with other symptoms as well, since the disease affects your entire body.
Early Signs of Rheumatoid Arthritis in Hands
Along with the stiffness, swelling, and pain you might notice in the joints of your hands, other symptoms can be early signs that the discomfort you’re experiencing might be rheumatoid arthritis. Look for signs like a low-grade fever, ongoing fatigue, and decreased appetite or weight loss.
Difference Between Osteoarthritis and Rheumatoid Arthritis
Arthritis is the overarching term referring to inflammation of the joints. But not all arthritis is the same—there are significant differences between osteoarthritis and rheumatoid arthritis. OA is a degenerative disease that affects primarily older people while RA is most common around middle age. Joint pain with OA often occurs on only one side—your right knee or left hand, for instance—while joint pain with RA is typically symmetrical.
While both osteoarthritis and rheumatoid arthritis come with some similar symptoms, like joint stiffness and inflammation, there are other signs associated with RA. Because RA is an autoimmune disorder, it affects body symptoms beyond just your joints and often comes with low-grade fevers, decreased appetite, and fatigue.
Is Rheumatoid Arthritis Hereditary?
While there are several contributing factors for RA, it’s common to ask: Is rheumatoid arthritis genetic or hereditary? The simple answer is that yes, studies show that genetics do increase your risk of developing the disease. Having a close relative with RA, especially a parent or sibling, ups your chances too. If it does appear in your family, you might want to ask your doctor about rheumatoid arthritis genetic testing. But know that having it in the family doesn’t guarantee you’ll have RA; heritability accounts for only about 20 to 50 percent of your odds of getting the disease, while other environmental and behavioral factors also play a large role.
Diseases Similar to Rheumatoid Arthritis
Rheumatoid Arthritis is notoriously tricky to diagnose, especially because the symptoms overlap with several other diseases, including:
Osteoarthritis comes with similar joint pain, stiffness, and swelling, though it typically only affects older individuals.
Gout is another form of inflammatory arthritis—but unlike RA, it usually affects only one or two joints, and symptoms are shorter lived.
Lupus is another autoimmune disease that can leads to swelling and pain in joints, but it typically also comes with a distinctive rash.
Lyme disease and fibromyalgia can also result in pain in soft tissues and joints.
Parvovirus is another with joint soreness and swelling that can be mistaken for RA; a blood test can confirm if you have parvovirus.
Rheumatoid Arthritis Symptoms
There’s a reason you’re often shown an illustration of a disembodied hand when discussing RA with your doctor! Rheumatoid arthritis most often hits the small joints of the hands and wrists first, where you may feel warmth, swelling, or tenderness. The joint pain of RA has been described in all sorts of ways—deep, dull, aching, throbbing, warm, hot, tender. However, most agree that the pain is typically worse in the early mornings. It can take at least 30 to 45 minutes for joints to loosen and feel better, and it generally worsens again after periods of inactivity.
That said, the signs of rheumatoid arthritis can also extend to your elbows, shoulders, knees, hips, ankles, feet, and neck. RA symptoms also tend to occur symmetrically; that is, joints on both sides of the body are usually affected at the same time. In some cases, other organ systems—including the eyes, heart, and lungs—may become inflamed too, leading to blurred vision, fluid build-up around the heart or lungs, along with chest pain and shortness of breath. (Right now, though, take a long, deep breath: RA is a serious illness, but complications can be controlled and even prevented. More on that below.)
Many people experience symptoms in lengthy episodes of days to years (it’s unpredictable like that), which may be separated by remission periods, when your RA symptoms subside. In fact, women with RA who are pregnant typically experience a complete hiatus of all RA-related symptoms through the pregnancy, because the hormones and immune system adjust to the state of the body. The symptoms usually return full force post-partum, as the body returns to its normal hormonal balance and immune-system functioning.
Early symptoms of RA may include:
Fatigue and weakness
Low-grade fever
General feeling of poor health
Loss of appetite and weight loss
Tight joints, usually on both sides of the body, that may be warm to the touch
With long-term, untreated rheumatoid arthritis, these additional symptoms may occur:
Stiffness (especially after waking up)
Hard—but painless—skin lumps, known as rheumatoid nodules, on the hands, elbows, knees, or toes that can range in size from a pea to a mandarin orange
Bent and misshapen joints
Dry mouth
Red, itchy eyes
Chest pain and breathing difficulty (in advanced cases where inflammation affects heart and lungs)
Reasons to See a Rheumatologist
What is a rheumatologist anyway, and what can a rheumatologist diagnose? They’re physicians who specialize in the treatment of arthritis and other conditions of the muscles, joints, and bones. Make an appointment with one if you're experiencing morning stiffness with any of the other early symptoms of RA, including fevers and weight loss. Or if you are not diagnosed, a primary-care doctor can refer you to a rheumatologist to run the necessary tests for rheumatoid arthritis. If you have rheumatoid arthritis and you experience a major flare or new symptoms, you should contact your rheumatologist or primary-care doctor to get help.
Rheumatoid Arthritis Diagnosis
RA is diagnosed based on your medical history, a physical examination, and laboratory and imaging tests (e.g., X-rays). Blood tests and other laboratory tests that may be used to help diagnose rheumatoid arthritis include:
Complete blood count (CBC): This common test is used to measure levels of red blood cells, white blood cells, and platelets in the blood. A low red blood cell count can be an indication of the chronic inflammation seen in.
C-reactive protein (CRP): Your blood is drawn, then checked for the presence of the CRP protein, which is produced by your liver during periods of inflammation and can be found in your blood in response. The normal range is approximately less than 1 mg/dL or less than 10 mg/L.
Rheumatoid factor: Also known as the latex agglutination test, this blood test is used to detect levels of this antibody, which are elevated in most patients who have RA.
Anti-cyclic citrullinated peptide (anti-CCP) antibody: Antibodies are proteins made by your body to fight off foreign substances. Anti-CCP is an antibody present in most RA patients. This simple blood test looks for the presence and level of the antibody.
Erythrocyte sedimentation rate (ESR): After a sample of your blood is added to a tube, a technician measures the rate at which the red blood cells fall to the bottom of the tube. A fast sedimentation indicates inflammation, with blood cells clumping together and falling quicker. Normal levels are less than 15 mm/hour in men and less than 20 mm/hour in women. Not everyone with RA has levels above average, but an elevated number can help your doctor confirm a diagnosis.
Anemia: Your doctor will look for anemia, or a low red blood cell count, which people with RA are at higher risk for.
Imaging scans and X-rays: Images produced from X-rays show the amount of damage that RA inflammation has caused in your joints.
MRI: Magnetic resonance imaging uses a magnetic field, radiofrequency, and computer technology to get quality images that are so sensitive, they can detect RA damage six months before it shows up on an X-ray.
Ultrasound: Sometimes referred to as ultrasonography, this is a very sensitive test that exposes both the bone erosion that happens in RA damage as well as the presence of inflammation.
Synovial fluid analysis: In this test, which is performed when a joint has pain, inflammation, or swelling, fluid is drawn from the joint to help determine a potential diagnosis. It could be an infection, gout, or arthritis, among other things. It’s important for docs to get this right because, obviously, gout—for example—has a completely different treatment plan than RA.
Rheumatoid Arthritis Treatment
There’s no cure for RA, but there are several treatment options to help you manage it. Your doctor will likely suggest a combination of therapies. Treatments have advanced greatly in recent years so patients are having better outcomes, less pain, and higher rates of remission. The goal of treatment is super simple: to keep you moving in all the ways you need to. That means reducing—and ideally stopping—the pain and inflammation that can eventually lead to joint damage. When RA is diagnosed early (check those symptoms!) and you’re aggressive with treatment, you're more likely to avoid complications later.
Treat-to-Target (T2T) is a newish treatment strategy that sets remission or minimal disease activity as the objective. How it works: Disease activity is frequently monitored and if the target (remission!) is not met, meds and doses are adjusted right then and there, at your appointment. How exactly? Docs follow a predetermined protocol, which could include medication, therapy, dietary changes, RA-friendly exercises, surgery, or a combination of treatment options.
Medication for Rheumatoid Arthritis
There are more rheumatoid arthritis medications and treatment choices now available than ever before, which makes it easier to find the best treatment plan for you.
RA medications include (listed, in general, in order of whether your RA is mild, moderate, or severe):
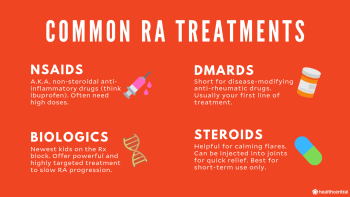
Nonsteroidal Anti-Inflammatory Drugs, or NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) do not slow the progression of RA, but your doctor may prescribe large doses of one to treat the chronic pain due to inflammation.
Common NSAIDs list:
Aspirin (Bufferin, Bayer)
Celecoxib (Celebrex)
Disalcid (salsalate)
Ibuprofen (Advil and other brands)
Naproxen (Aleve and other brands)
Relafen (nabumetone)
COX-2 inhibitors, a subclass of NSAIDs that have a lower risk of internal bleeding or stomach ulcers—a common side effect of other NSAIDs that are used in large doses for a long time. If you do need high doses of those other NSAIDs, it should be a short-term fix.
DMARDs
These disease-modifying anti-rheumatic drugs (hence: DMARDs) help preserve joints by blocking inflammation. Unlike treatments that only address your symptoms, such as NSAIDs, DMARDs go to the root of the problem to slow down your RA and can even cause remission. Some DMARDs were originally used for other medical conditions, like malaria or cancer, and then were found to be effective treatment for RA. Due to the unpredictable risk of potential side effects from DMARDs—such as upset stomach, infection, hair loss, and liver damage—you must be closely monitored with regular (weekly to every few months) lab tests when taking these medications.
Trexall (methotrexate)
Azulfidine (sulfasalazine)
Arava (leflunomide)
Plaquenil (hydroxychloroquine)
Imuran (azathioprine)
Janus kinase (JAK) inhibitors
Biologics for RA
Also known as biologic response modifiers, these medications are designed to control certain parts of the immune system—in fact, they’re a type of antibody. But instead of locking onto bacteria or a virus, they target, then shut down, the proteins that fuel inflammation. (Cool, right?) Today, there are many different biologics available, so doctors categorize them based on the cells they put a bull’s-eye on.
Tumor necrosis factor inhibitors (TNF-inhibitors), or tumor necrosis factor blockers—such as Humira (adalimumab), Enbrel (etanercept), Cimzia (certolizumab), Simponi (golimumab), and Remicade (infliximab)—put the brakes on tumor necrosis factor, a naturally occurring substance that is overproduced in people with RA; it’s the main cause for the first inflammation a person with RA gets. They’re delivered by self-injection or IV infusion, depending on the drug. Possible side effects include:
Upset stomach
Nausea
Headache
Increased risk of infection, such as upper respiratory, skin, or vaginal
B-cell inhibitors, like Rituxan (rituximab), are administered through an IV and kill B-lymphocytes that can spark inflammation.
Interleukin-1 (IL) blockers, like Kineret (anakinra), are self-injected daily; they target interleukin-1, an inflammatory compound in the body.
Interleukin-6 inhibitors, such as self-injected Kevzara (sarilumab) and IV-administered or self-injected Actemra (tocilizumab), stop interleukin-6 proteins from attaching to cells and triggering inflammation.
T-Cell inhibitors, like Orencia (abatacept), latch on to the surface of T-cells (aka inflammation-causing white blood cells). A doctor will give you this medicine via IV.
Oral corticosteroids, such as Deltasone (prednisone), offer quick relief from symptoms of rheumatoid arthritis and, in advanced cases, can prevent RA-related inflammation from harming your eyes and internal organs. Because prednisone has serious side effects when used for extended periods, it is often reserved for severe flare-ups or when other treatments are ineffective. Injections of corticosteroids into an affected joint may also be helpful.
Steroids
Oral corticosteroids, such as Deltasone (prednisone), offer quick relief from symptoms of rheumatoid arthritis and, in advanced cases, can prevent RA-related inflammation from harming your eyes and internal organs. Because prednisone has serious side effects when used for extended periods, it is often reserved for severe flare-ups or when other treatments are ineffective. Injections of corticosteroids into an affected joint may also be helpful.
Surgery
There are some RA cases—usually advanced and/or undertreated—where surgery may be a necessary consideration. Meaning: The pain is likely debilitating, and you no longer have normal joint function. There are two surgery types:
Synovectomy
Any time swelling has gotten so bad that you’re having a hard time moving and functioning, this surgery may be performed. It removes the diseased synovial membrane from affected joints to reduce swelling and pain and help prevent further joint damage.
Arthroplasty
This surgery replaces the damaged joint with a mechanical one to restore joint function or fix a deformity. More than a million joint replacement surgeries are performed each year, mostly of the hip or knee, but the shoulders, elbows, and joints in the hands and feet may be replaced as well. Critical to discuss with your surgeon: the types of activities you want to continue after joint replacement. This will help your doc select the appropriate type of prosthesis and implantation technique, while giving you a deeper dive into the risks and limitations of surgery.
Natural Remedies for Rheumatoid Arthritis
If you have RA, yes, you have a chronic illness. But there are number of things you can do—in addition to typical meds—to help you feel your best. For this, consider assembling a medical team of specialists from a variety of fields, including psychiatry, nutrition, and radiology. Other health-related professionals may also be part of your team to assist you with the following:
Exercise
Staying active doesn’t have to be off the table if you’re diagnosed with RA. Your doctor may prescribe an exercise program or advise you to see a physical or occupational therapist. While exercise that is too vigorous may worsen your symptoms, programs with gentle exercises can increase the range of motion of your joints. You may also need to modify certain moves depending on your mobility and if you’re in any pain. Some exercises are done with equipment you can keep right at home, others are easier to perform in a pool or hot tub because water helps support the body. Talk to your doctor about which techniques would be best for you.
Sleep
Given how uncomfortable the condition is, more than half of people with RA have trouble sleeping at night. Of those people, 25% to 40% report sleep disturbances related to their RA. Plus, RA-related inflammation tends to deplete energy levels faster than for those without RA—so a solid eight hours of shut-eye is even more critical. Start tonight by using pillows as extra support where needed (for example, under a painful shoulder or between stacked knees).
Hot/Cold Therapy
Since heat works to reduce muscle tension and stimulate blood circulation, many people with RA say that applying something warm (a fresh-from-the-dryer hoodie will do!) makes joints feel better before exercise and other physical activity. Cold compresses, on the other hand, reduce inflammation, swelling, and soreness after an RA flare. And both heat and cold can be a quick fix to ease achy hands.
Relaxation Techniques
It’s easier said than done, yes. But with the association of rheumatoid arthritis and stress (86 percent of patient says it’s the most frequent cause of joint symptom flares), whatever you can do to take it easy can be more than an emotional relief. You might try meditating, do yoga, see a therapist—whatever works to help you find a sense of calm can ease your aches, too.
Rheumatoid Arthritis Topicals
Applying creams or lotions containing capsaicin (an extract from chili peppers!) may soothe minor joint pain. Ditto for those with camphor, menthol, or turpentine oil. Try: capsaicin-infused Capzasin HP Crème or J.R. Watkins White Cream Liniment, which has both camphor and turpentine oil.
Compression Therapy
There are several specialty clothing items with a snug fit that can help provide some relief from RA pain. Look for compression gloves, hose, and socks. In addition, your rheumatologist may prescribe splints for areas that are trouble spots for you. For instance, you might find relief from a finger splint, hand splint, resting hand splint, wrist splint, or ring splint for rheumatoid arthritis. During severe episodes, they'll help relieve pain by immobilizing your joints.
Rheumatoid Arthritis Diet
The truth: There is no single diet that will cure your RA, or even come close. But good nutrition can help with inflammation, which in turn may ease some symptoms. While most evidence about the role of diet with RA is anecdotal, there are some studies that indicate certain foods may be helpful.
The Mediterranean diet (aka the anti-inflammatory diet)—which emphasizes fish, olive oil, and vegetables—has been shown to have some impact on inflammation, likely due to the omega-3 fatty acids in certain fish.
A vegan or vegetarian diet can also be helpful for RA symptoms, according to several smaller studies. Learn all about RA and diet here.
Types of Rheumatoid Arthritis
There are a few different ways RA can express itself. These are the most common types of rheumatoid arthritis:
Seropositive Rheumatoid Arthritis
In RA, there are two classic auto-antibodies: rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP). If you have RA and test positive for auto-antibodies, you have seropositive rheumatoid arthritis—which affects about 70% to 80% of RA patients.
Seronegative Rheumatoid Arthritis
If you have seronegative RA, blood tests don’t show the RA at all and tests can be inconclusive. While symptoms between seropositive and seronegative RA are similar, some research suggests seronegative patients have a lower risk of joint damage.
Juvenile Idiopathic Arthritis
Although rheumatoid arthritis most commonly affects people between ages 30 and 50, it can strike at any age. Juvenile idiopathic arthritis is a type of the inflammatory autoimmune disease that affects children before age 16. Like other forms of RA, it affects the joints and has several other health outcomes as well.

Rheumatoid Arthritis Flares
Thankfully, the symptoms of RA are not constant. You’ll likely have times when it doesn’t bother you and others, known as flare-ups or flares, when the pain can be debilitating. Like a tornado, the triggers of rheumatoid arthritis are unpredictable. The best way to gain more control? Pinpoint the culprits behind your flares. Everyone’s are different, but typical offenders include:
Stress
Infections, including flu and cold, that activate your immune system
Physical trauma, like surgery or broken bones
Post-pregnancy
Poor dental health
Certain foods, including processed snacks, red meat, and excess refined sugars
Too much exercise
Dramatic, sudden changes in weather
Rheumatoid Arthritis Complications
It can. Side effects from rheumatoid arthritis are manifestations of the condition itself and come in two varieties: those from untreated or undertreated RA, and those caused by joint damage. Common complications of RA of RA include:
Dry eye. This is the most common eye complaint for people with RA.
About 10% of people diagnosed with RA (and diligently treated) experience complete remission within one year, and roughly 40% go into remission within two years. That’s thanks to significant advances in treatment over the past two decades.
Heart disease. It affects more than half of all people with RA.
Rheumatoid nodules, which occur in 30% to 40% of RA patients and are more bothersome than painful.
Osteoporosis-related fractures. These are 25% to 30% more common in people with RA than the general population.
Infections (flu, staph, pneumonia). They’re twice as common in people with RA.
Lung disease. It develops in nearly one-fourth of RA patients.
Additional complications from RA may include:
Anxiety
Carpal tunnel syndrome
Cervical myelopathy
Depression
Diabetes
High blood pressure
Inflammation
Obesity
Stress
Tendon rupture
Susceptibility to infections
Vasculitis
This is exactly why it’s so critical not to ignore symptoms—or to put off getting help. If the disease progresses and is not treated, that’s when the worst side effects can occur: severely restricted range of motion or, worse, gradual destruction of the joints. The inflammatory process slows down as fibrous tissue forms or bones fuse, and joints stop functioning altogether.
Rheumatoid Arthritis Flare Prevention
While there is no known way to keep from getting rheumatoid arthritis, there are plenty of steps you can take to prevent complications and help lessen the impact of a flare.
Quit smoking. A Swedish study of 34,101 women reported that even light cigarette smoking is associated with increased risk of RA in women and that quitting (or not starting at all) may reduce the risk.
Maintain a healthy weight to ease pressure on your joints. If you are overweight, you may want to consider a weight-loss plan, as excess pounds c:n put unnecessary stress on your joints. Consider working with a dietitian to help build a personalized diet or program that targets your specific goals (i.e. less sugar and more omega-3 fatty acids/fish) for managing your RA.
Eat a healthy diet. While there is no prescribed diet for RA, aim to avoid foods that cause inflammation, like packaged snacks,and include foods that promote bone health and immune function.
Start or keep up with an exercise routine. Research shows that exercise can help alleviate RA symptoms and even improve day-to-day functioning. It can also make you more flexible, help you sleep better, and boost your endurance.
Stress less. Research published in Annals of the Rheumatic Diseases found a link between having a major psychological stress (think: job loss, death, divorce, etc.) and having more active RA disease. Incorporating effective stress-reduction techniques like deep breathing, mindfullness, and therapy, could be a huge benefit to your treatment protocol.
What’s Life Like for People With RA?
A day-to-day with rheumatoid arthritis often includes pain and fatigue, which can, admittedly, be overwhelming. You may also have to deal with people who don't really understand your condition and can't fully grasp what you're going through. If RA is relatively new to you, or you’re exhausted and in constant pain, we understand how impossible it can feel to gather the strength to search for good care and try new treatments. So start small: First educate yourself about RA, then work toward building confidence in who you are as a person living with RA.
Emotional Health
People who have rheumatoid arthritis often feel that they must mask or disguise their issues, which can be a real drain on your brain. The best solutions?
Speak up. Simply talking with friends and family about what you're going through with RA can remove that burden of solitude—and help your people help you in the way you need it.
Find ways to relieve stress. Try creating a self-care routine and exploring alternative treatments like meditation.
Consider talking to a therapist. Being diagnosed with RA often triggers a grieving process as you mourn the healthy you and work toward acceptance of your situation. You may feel depressed, particularly if your disease is super active. By prioritizing your mental health and linking up with a counselor or therapist (your family doc or rheumatologist can refer you to one), you will set yourself up to follow through with all other aspects of RA management.
Sex Life
Fifty-nine percent of those with RA, per a study published in Rheumatology, felt the disease had a negative effect on their sex life. And no wonder: Depending on its severity, RA itself—along with some of the meds used to treat it—can decrease desire due to fatigue, stiffness, vaginal dryness, erectile dysfunction, and a decreased libido.
So, what’s the fix? Patience, communication, and understanding between you and your partner are obviously key. There are also certain sex positions that may feel more comfortable for you, typically based on your most ouchy joints:
For wrist and/or elbow pain: Lie on your back or side, and place pillows under your elbows as needed.
For neck pain: Don’t put pillows behind your neck or bend it forward when you’re on your back having sex. And be sure to talk to your doctor about how RA may affect your neck and how to protect it.
For hip pain: If it hurts to move your hips around, have sex in a spoon position, with your partner behind you.
For knee pain: You want to keep your knees straight, so try being on the bottom in the missionary position or lie on your sides facing each other.
Pregnancy
It’s complicated enough without RA—so of course getting pregnant with the condition comes with a billion extra questions. Will I have to come off my medication? (There are some medicines that are unsafe to take during pregnancy, while others are fine.) Will I pass RA on to my children? (In short, not necessarily.) Learn as much as possible about the issues to consider, and talk to your rheumatologist early on (ideally, before you start trying) regarding medication risks.
Where Can I Find Rheumatoid Arthritis Communities?
RA affects such a small percentage of the population that, without actively searching, running into another RA-er IRL is as likely as spotting a Charleston Chew at a movie-theater concession stand. Yet, finding your people—those who know exactly what you’re going through—is just as important to your mental wellbeing as finding a treatment plan that works. Form connections, discover resources, share both pain and inspiration, and make new friends, starting here.
Top RA Instagrammers
Desiree Lee, @thebarbellbeautie
Follow because: She may be afraid of needles (hello, Humira shots), but she is not afraid of a barbell. Serving up your daily dose of workout inspiration—and actual workout routines—without ignoring the exercise issues that come with a chronic condition.
Renee Anderson, @the_rheumatoid_arthritis_mama
Follow because: She’s relatable on every level: She covers all aspects of how RA affects her life—and shares that emotional rollercoaster in her captions—including how she maintains a robust marriage in a hurting bod, keeps mommin’ through exhaustion, and fuels her health with arthritis-approved recipes.
Eileen Davidson, @chroniceileen, chroniceileen.com
Follow because: She’s a mega-advocate who is hellbent on making her rounds to raise awareness about what it’s really like to have RA, and she makes no (sore) bones about it. She’s a born storyteller, with a side of sass.
Top RA-Related Podcasts
Chronic Briefs. By versatile and hilarious writer Daniel Malito (who has had juvenile arthritis for more than 25 years, since he was 11 years old), the archives of this RA-related podcast are poignant and sometimes LOL-funny.
Chronic Sex. Sex educator and activist Kirsten Schultz hosts this explicit—as in, NSFW unless you’re wearing headphones!—podcast, uncovering truths about how chronic illness and disability (including RA) affect relationships, sex, and sexuality.
Sickness + Health. Artist and health advocate Cara Gael O’Regan has lived with Ehlers-Danlos Syndrome, another joint-related condition, for more than two decades; here, she does in-depth interviews on some of the toughest topics—insurance coverage, disability, mortality—as they intersect with chronic conditions and pain.
Arthritis and Work by the Arthritis Society. While it’s not an ongoing series, this is a gold mine of solid work-related resources specific to balancing a career when you have RA.
Top RA Support Groups and Non-Profits
Arthritis Foundation. This org and its award-winning magazine, Arthritis Today, help you create a personalized plan for a full life. From quizzes (“What’s Your Arthritis Diet?”) and expert Q&A’s to customizable programs and tools (“Track and React,” a symptom-tracking app), the Arthritis Foundation encourages you to look at your RA diagnosis holistically.
The Arthritis National Research Foundation. For more than four decades, this group has provided grants and organized fundraising for arthritis research into the causes and prevention of, and new treatments for, chronic joint conditions. Whether you're heavy into science or not, this is where you'll want to look for researchers’ latest and greatest RA findings.
CreakyJoints is a digital community for arthritis patients and caregivers to find education, support, advocacy, and resources. Their programming and services are free and they offer a ton of articles and first-person stories about various types of arthritis. CreakJoints is basically one-stop shopping for connecting with patients and experts in the joint-health space.
Rheumatoid Arthritis Support Network. Its goal? Provide up-to-date information so that people with RA know their options for prescription drugs and alternative therapies, and fully understand their diagnosis. The site also has a treasure trove of resources, including a rheumatologist directory.
My RA Team. This massive social network virtually connects you with others who have rheumatoid arthritis. It’s great for emotional support, practical advice, and real-world insights on managing the condition.
Additional reporting by Laurel Leicht.
Sure, they might look—and even feel—very similar, but the difference is in the cause. OA is the result of years of wear and tear (see great-grandma’s bulging knuckles). RA, on the other hand, is strictly autoimmune, meaning you get it when the immune system wigs out and instead of attacking infection and bacteria, it targets healthy cells and tissues.
People with RA are twice as likely as those without it to get coronary artery disease (CAD). While the consensus is still out on the main cause for this correlation, many cardiologists believe that chronic inflammation works with other factors like abnormal cholesterol levels to increase the risk of heart problems.
The typical presentation of early RA includes joint stiffness in the mornings lasting for more than 30 minutes, and pain and swelling in the small joints of the hands or feet. Some of the atypical symptoms include fatigue, low-grade fever, and dry eyes.
No two people will feel the exact same thing, but in general people start off feeling a warm or even burning sensation around the affected joints as well as a stiffness that makes movement slow. Over time, untreated inflammation can damage cartilage and bones. The space between bones can become smaller, leading to unstable, painful. Eventually, inflammatory tissue begins to build up, sometimes causing tender nodules to form around the area.







