How Doctors Diagnose Rheumatoid Arthritis
When you’ve got aches in your joints that just won't go away (and no, they're not the kind of "pop an aspirin and you'll fee fine" type, either), it's probably time to get things checked out. The best place to start? With your GP. Your doc will ask about your symptoms and medical history, then order several tests that can help determine whether you have rheumatoid arthritis (RA), osteoarthritis (OA), or something else entirely. “Usually when you see your primary-care provider, they know which initial tests need to be ordered and then make appropriate referrals [to the rheumatologist],” says Sadia Khan, M.D., a rheumatologist at Mercy Medical Center in Baltimore.
Why ID-ing RA Is Key
Identifying whether you have arthritis and, if so, which type it may be is crucial because each form of arthritis has different causes and treatment options. RA is a systemic autoimmune disease that targets the joints and causes body-wide inflammation, while osteoarthritis is a non-inflammatory condition that causes cartilage loss in the joints, either from trauma or overuse. Both conditions are painful, but for pretty different reasons, which means how your doc treats your symptoms will vary. Keep reading to learn how your M.D. may diagnose you with RA.
Step 1: Finding Out Where You Ache
“The first symptoms people with RA report are most often pain, swelling, and stiffness of the small joints in the hands and feet,” says James Cohen, M.D., a rheumatologist with Indiana University Health in Indianapolis. People with rheumatoid arthritis also typically experience symmetrical swelling and pain, meaning that both hands or feet are affected. If you only have pain in joints on one side of your body, it’s less likely to be rheumatoid arthritis and more likely to be osteoarthritis, caused by cartilage damage.
Step 2: Learning When You're Stiff
RA-related stiffness is usually worst in the morning and lasts about an hour, Dr. Khan says: “The fingers are tight. They have a hard time moving–they feel like the Tin Man–and then as they get moving, in half an hour to an hour, symptoms get better.” Any extended period of sitting or just not moving can cause RA joints to stiffen up, too. Osteoarthritis stiffness typically happens for less time later in the day, after physical activity.
Step 3: Reviewing Your Risk Factors
Your doctor may suspect you're dealing with rheumatoid arthritis if you’re a woman because about 75% of people who are diagnosed with RA are female. Some women are diagnosed with RA early, in their 20s or 30s, but a number are diagnosed later, in their 50s or 60s. (It's also possible to be diagnosed with a childhood form of the disease, known as juvenile idiopathic arthritis, or JIA.) Men who are diagnosed tend to be older. If you have first-degree family members (parents, siblings or children) who have been diagnosed with RA, tell your doctor, because that increases your risk as well.
Step 4: Discussing Other Symptoms
Although symmetrical joint pain and swelling are the hallmarks of rheumatoid arthritis, it’s a full-body disease that can cause full-body symptoms. Along with mental health issues, including anxiety and depression, sometimes people experience loss of appetite, exhaustion, low-grade fever, and even nerve damage, says Dr. Cohen. Neuropathy—the term for muscle weakness, numbness, or a pins-and-needles sensation—may be another clue that rheumatoid arthritis is the culprit. Osteoarthritis, on the other hand, is much more of a localized condition.

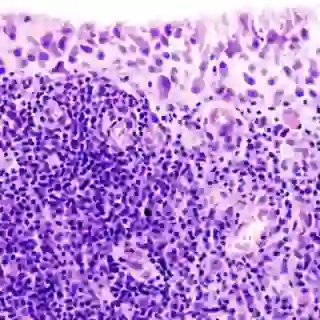
Step 5: Ordering Imaging Tests
Rheumatoid arthritis impacts the lining of joints, which eventually leads to the damage of joint tissue. Your doctor may order x-rays to check for joint damage caused by RA. (On the other hand, if you're dealing with osteoarthritis, x-rays may show signs of cartilage loss or bone spurs.) Sometimes, doctors order CT scans, ultrasounds, or even MRIs. “X-rays in early stages of rhematoid arthritis may not show the changes,” caused by the disease, Dr. Khan says. “Ultrasound and MRI give far more information about the joint lining and whether or not the tissues around the joints are inflamed.”

Step 6: Running Lab Tests
Your doctor may offer blood tests looking for rheumatoid factor (RF) and/or anti-CCP (anti-cyclic citrullinated peptide) antibodies to diagnose rheumatoid arthritis, even though these tests aren't always definitive. Some people with early-stage RA or other autoimmune diseases may have false positives or negatives. Sometimes, getting tested again several months later may show a different result. “About two-thirds of the time, rheumatoid arthritis can be diagnosed based on blood tests and symptoms,” Dr. Khan says. Being CCP-antibody positive is generally more indicative of rheumatoid arthritis; the RF test tends to draw more false positives.

Step 7: Running More Tests
Doctors will also likely measure your overall level of inflammation using two common tests: C-reactive protein (CRP) and the erythrocyte sedimentation rate (ESR). Not everyone with rheumatoid arthritis has elevated levels, but when the numbers are high, the findings can help confirm the diagnosis. “If a patient has elevated ESR and/or CRP levels, it would imply they have an inflammatory kind of arthritis, versus osteoarthritis,” Dr. Cohen says. Your doctor may continue to use these tests to monitor your disease and inflammation levels over time.
The Importance of Early Diagnosis
A generation ago, it mattered far less whether you were diagnosed with rheumatoid arthritis in its easliest stages or further down the proverbial funnel: There were no meds regardless to halt its progression with any great success. But today, when RA is caught and controlled early enough, you may never experience complications like joint damage or changes. That’s why it’s so important to “see your doctor at the first signs of RA—joint pain, warmth and swelling around the wrists and knuckles, and morning stiffness that lasts for more than 15 minutes,” Dr. Cohen says. You did the right thing by taking action.

Find a Treatment Plan That Works
Although there is no cure for rheumatoid arthritis, “Medicine and treatment for RA have advanced a lot over the past few years, and we can likely prevent or stop the progression,” says Dr. Cohen. Doctors typically prescribe disease-modifying antirheumatic drugs (DMARDs), which can alleviate symptoms and slow RA down. Sometimes, people are also prescribed nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to help with pain and inflammation. And some patients receive biologics, which help prevent inflammation and joint damage in more serious cases. You’ve got lots of options!
-
RA and Imaging: National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2019.) “Diagnosis of Rheumatoid Arthritis.” niams.nih.gov/health-topics/rheumatoid-arthritis/advanced#tab-diagnosis
-
RA and Risk Factors: Arthritis Foundation. (n.d.) “What Is Rheumatoid Arthritis?” arthritis.org/about-arthritis/types/rheumatoid-arthritis/what-is-rheumatoid-arthritis.php
-
RA and Treatments: American College of Rheumatology. (2019.) “Rheumatoid Arthritis.” rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Rheumatoid-Arthritis