Psoriasis: Everything You Need to Know
We've got the doctor-approved details on psoriasis causes, symptoms, treatments, and a jillion other facts and tips that can make life with this skin condition easier.






Whether you’ve just been diagnosed or worry you could have psoriasis, you’re probably nervous, confused, and maybe even a little scared. That’s normal, and everyone featured on HealthCentral with a chronic illness felt like you do now. But we—and they—are here for you. On this page alone, you’ll discover the realities and challenges of the condition, but also the best treatments, helpful lifestyle changes, where to find your psoriasis community, and all the crucial information to help you not just manage—but thrive. We’re sure you’ve got a lot of questions...and we’re here to answer them.
What is Psoriasis, Anyway?
There’s a reason the P is silent in psoriasis. This condition, which impacts 8 million Americans, is mighty sneaky. Psoriasis is an immune-related disorder that affects the body’s largest organ—the skin—causing lesions that can range from small red bumps to thick, raised lesions to lobster-like redness from head to toe. Some people with psoriasis say that the lesions burn, sting, or itch. (And unfortunately, while a temporary relief perhaps, scratching can worsen psoriasis and trigger more flares.)

To understand those lesions, you need to go below the surface. Psoriasis stems from an overactive, uber-sensitive immune system. Even though there is nothing to see or feel here (keep moving along, please!), the immune system rings the false alarm, causing your skin cells to grow far more quickly than they should.
No blood test or urine sample can diagnose psoriasis. Your dermatologist or M.D. will spot it on looks alone. And while psoriasis doesn’t discriminate by sex (it strikes men as often as it does women) or age, it’s much less common in the playground set. The peak period for occurrence between the ages of 15 to 35 years old.
What Causes Psoriasis in the First Place?
Genetics deserve a mug shot in the police line-up. An estimated 10% of people are born with at least one of the genes that predisposes them to psoriasis. (Researchers believe there are about 25 genetic variants that make you more susceptible to developing psoriasis.) The condition is more likely to occur if a direct relative (parent, grandparent, sibling) has a history. If Mom or Dad has psoriasis, you’ve got a 14% chance of developing it. If both do, your chances spike to 40%. That said, many experts say that you need both a genetic component and an exacerbating factor (listed below), to trigger a psoriasis outbreak or chronic psoriasis.
A cold, strep throat, earache, bronchitis, or respiratory infection
Use of a medication such as lithium, antimalaria medications, Inderal for high blood pressure, the heart medication Quinidine, and a nonsteroidal anti-inflammatory used for arthritis called Indomethacin
Withdrawal from a steroid like Prednisone
A skin injury or trauma such as a sunburn, scratch, even a bug bite, and areas where a vaccination or tattoo has been received (when psoriasis lesions occur at nontypical sites like these, it’s called a Koebner phenomenon)
Stress, both positive (preparing for your wedding) or negative (getting in an accident)
Google it, and you’ll find lots of alarming factors such as weather, allergies, and diet—but none of these have been proven in studies. Some research, however, shows that being overweight or obese bumps up your chances of developing psoriasis and once you have it, being overweight or obese can exacerbate your symptoms. One study found that overweight or obese patients who go on a highly restrictive diet—about 1,200 calories a day—can ease psoriasis symptoms. But more research is needed.
What Are the Types of Psoriasis and Do I Have Symptoms?
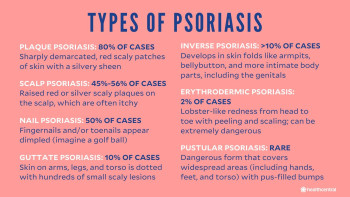
Like biblical sins and the Earth’s seas, there are seven types of psoriasis—well, says us (and many doctors). While The National Psoriasis Foundation counts five official types, given that nail and scalp psoriasis can occur on their own (less common) or in conjunction with other types like plaque (more common), we think seven is justified.
Each type is defined by the appearance of the lesions or their location, and so the symptoms will differ. Let’s break ’em down from most common to least.
Plaque Psoriasis
If you are diagnosed with psoriasis, odds are you have plaque psoriasis. It’s the most common type at 80% of cases and characterized by sharply demarcated, red scaly patches of skin called plaques. The peaks of these plaques will have a silvery sheen, though in dark skin they can look purple.
Plaque psoriasis is a chronic condition for about 90% of those diagnosed with it. The lucky 10% have what’s called “spontaneous remission,” where your skin unexpectedly clears up for good. While it commonly shows up on specific areas like the elbows, knees, scalp, and intergluteal cleft (the groove between the buttocks), these plaques can appear anywhere on the body—though scalp psoriasis accounts for 50% of plaque psoriasis cases.
Scalp Psoriasis
Scalp psoriasis typically occurs with plaque psoriasis but can crop up with other types as well. In fact, 45 – 56% (mighty specific range, we know) of psoriasis sufferers have scalp psoriasis. However, it can also surface on its own without any other type. The raised, red, or silver scaly plaques appear on the scalp where they can be itchy and painful and may shed on your hair, clothes, or furniture. Unlike dandruff, the scalp will be inflamed, maybe even bleeding.
Nail Psoriasis
Of all the people who suffer from psoriasis, up to 50% will have nail psoriasis. Like scalp psoriasis, it typically occurs with plaque psoriasis but can rear with other types as well. It can also appear on its own without any other type. What does it look like on fingernails and toenails? Golf ball dimples or depressions, ridging, thickening, and discoloration. In severe cases, nail psoriasis can cause deformation, crumbling, or detachment of the nail from the nail bed.
Guttate Psoriasis
Guttate psoriasis affects about 10% of those with psoriasis, appears as scaly, dotty lesions smaller than a fingertip. You can get hundreds—yes, hundreds—of them, typically on your arms, legs, and torso. The upside is that guttate psoriasis is commonly triggered by infections, like strep throat, and once you treat the psoriasis, it usually goes away and doesn’t come back.
Inverse Psoriasis
Inverse psoriasis affects fewer than 10% of people with psoriasis and lives in the folds of skin. Think: the armpits and bellybutton, but also more intimate body parts such as the genitals.
Pustular Psoriasis
Pustular psoriasis is a rare, dangerous form of psoriasis that covers widespread areas like hands, feet, and the torso with superficial pus bumps and scaling. The spots may seem infected, but they’re not. We repeat: They are not. The real danger here is you’re losing the protective function of the skin, which means heat, water, and electrolytes escape the body. Not to freak you out, but this can be deadly. It usually develops quickly and suddenly. If you experience this kind of psoriasis, get medical attention ASAP.
Erythrodermic Psoriasis
Erythrodermic psoriasis is the rarest of all types affecting only 2% of psoriasis sufferers. It causes lobster-like redness from head to toe, peeling, and scaling. Similar to pustular, it severely compromises the skin’s protective functions so, again, see a doctor immediately if you experience this.
What Is The Best Treatment for Psoriasis?
Sorry, but we need to answer that Q with a few more Qs: How is your overall health? Are you pregnant or do you have cardiovascular disease? Is the psoriasis on a small or large area? Where does it appear on your body?
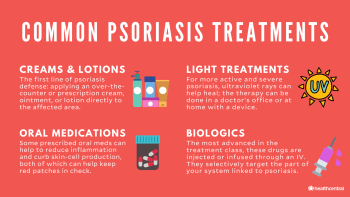
This is our way of saying that there is no single best psoriasis treatment for everyone. But a variety of options can help minimize both the impact of this chronic disease, its progression, and its side effects. Here are some treatment choices for psoriasis:
Over the counter or prescription topical creams, ointments, and lotions are applied directly to the affected area. Best for mild psoriasis, this category includes topical corticosteroids, Vitamin D, retinoids, and salicylic- or tar-based products, the latter two are particularly helpful in scalp psoriasis.
Ultraviolet light treatments are the go-to for more active and severe psoriasis. The most commonly used is narrowband UVB, usually done in a doctor’s office or at home with a phototherapy device. It typically requires 2 to 3 treatments a week for about eight to 16 weeks. Although it works on all skin colors, one risk is dark spots on those with medium to dark complexions.
Excimer laser therapy is another light-based treatment that’s best for mild to moderate psoriasis in smaller areas. An excimer laser emits high intensity UVB light of a specific wavelength on psoriasis plaques.
Oral medications, such as methotrexate and cyclosporine, reduce inflammation or curb skin cell production. These medications are mildly to moderately effective but have side effects, and not minor ones either (nausea, hair loss, high blood pressure, and kidney problems), so newer medications called biologics (see below) are often used instead.
Biologics, drugs produced from living organisms, are usually injected into the body or given through an intravenous drip and selectively target the parts of the immune system associated with psoriasis. According to a November 2021 report from M Health Lab, it can be tough to predict which PsO patients will have a robust response from injectible TNF inhibitors, which are biologics that work to tame inflammation. One recent study published in the Journal of Allery and Clinical Immunology suggests that changes of specific gene expressions in healthy skin (as opposed to active plaque flareups) during and after such treatment can provide important clues about whether or not this approach might be right for you. (In other words, there may be an underlying genetic component that could affect the drug's success.)
If one treatment doesn’t work, it doesn’t necessarily mean it’s time to try another. Instead, your doctor may adjust your dosage and the frequency of your treatment. Trial and error and patience are important. But only for so long. That’s why the National Psoriasis Foundation says that the psoriasis should cover 1% or less of your body within three months. If that benchmark isn’t reached, you and your MD can reevaluate your plan.
Does Psoriasis Have Serious Complications?
We can’t mince words. Yes. Having psoriasis increases your risk of other health issues—mental and physical. The risks and complications that may come with psoriasis include:
Depression. Your risk is twice as high as in those who don’t have psoriasis. The reason? Twofold, actually. Experts suggest that the physiological changes you undergo with developing psoriasis may also lead to depression. In addition, you may feel self-conscious of skin lesions and the attention they may draw from other people, leading to emotional distress.
Stroke. Researchers are trying to connect the dots between psoriasis and cardiovascular disease. Your risk of a stroke is 43% higher had you not had the skin disorder. Big asterisk here, though: The risk is greatest in those with severe cases of psoriasis. If you fall into that camp, it’s crucial to work with your doctor on monitoring lifestyle habits such as smoking.
Psoriatic arthritis. About 30% of psoriasis sufferers also have psoriatic arthritis, a chronic condition that’s also deeply linked to the immune system. While psoriasis affects the skin, psoriatic arthritis affects the joints and some parts of the body where ligaments and tendons are attached to the bone. The result is stiffness, swelling, pain, and joint damage, which in some cases can be irreversible. A vast majority (85% to be precise) develop skin psoriasis first and then the joint version crops up years—even a decade—after psoriasis is diagnosed. In fact, if you have psoriasis and your joints begin to stiffen, your doctor will suspect psoriatic arthritis. (Case in point: Kim Kardashian was recently diagnosed with psoriatic arthritis—13 years after her first flare up of skin psoriasis.) As with psoriasis, psoriatic arthritis can flare at any age, but its peak time is between ages 30-50. Although some treatments for psoriasis can alleviate psoriatic arthritis symptoms, it’s best to see a rheumatologist, an M.D. who specializes in arthritis.
Lymphoma and nonmelanoma skin cancer. If you have psoriasis and psoriatic arthritis, your risk of lymphoma and nonmelanoma skin cancer is higher than if you don’t have these conditions. Doctors are unsure whether the link is due to the inflammation caused by the conditions themselves (it’s been linked to the growth of cancer), or from medications that impact the immune system.
Osteoporosis. While exact numbers are not available, one small study found that 18% of study participants with psoriasis had the bone disease, while an astounding 60% had osteopenia, a precursor to osteoporosis. The sooner you catch this, the better. Researchers found that the threat increases by 5 percent for every year the bone disorder goes unnoticed.
What's Life Like for People with Psoriasis?
Psoriasis may be diagnosed by a doctor’s eyes alone, but living with the condition impacts all the senses—sight, touch, and even taste, as your diet may need to be overhauled.
Physical Health
Psoriasis can be itchy and painful. And depending on your treatments, the side effects are not fun, and can include: joint pain, high blood pressure, and nausea. We can’t underscore enough how crucial it is to work closely with your MD to find the treatment plan that gives you the most extensive skin clearing with the fewest side effects. And as we just mentioned, because psoriasis is linked to cardiovascular and bone health, it’s crucial for those suffering from the condition to rethink their diet.
Emotional Health
This is a condition that largely doesn’t hide—it lives on the exposed areas of your face, scalp, elbows, and knees. The patches tend to come and go, but it can be disheartening (even cringe-worthy) when a flare up occurs, or when scaly skin sloughs off and lands on your clothes or furniture. Singer Cyndi Lauper has said about her plaque psoriasis that, at its worst, when it covered much of her body, she stopped working and stayed in bed. Kim Kardashian has also been public about her psoriasis struggles, talking openly about times when plaques covered much of her face and body. Being diligent with your treatment plan can certainly help clear your skin. But if you’re feeling stressed and fear an outbreak, there’s anecdotal evidence that mind-mellowing routines such as meditation, exercise, or long baths can do the trick. Support groups that foster interpersonal communication can ease the mind as well.
Sexual Health
People with psoriasis often feel self-conscious in public. That discomfort can double with sex. Before you’re close to getting intimate, try talking openly about it with your partner. Tell him or her what it is and that it’s not contagious or infected (even if it appears to be). For those with psoriasis on or around their genitals, sex can be emotionally and physically painful. (This can affect 30%–60% of people with psoriasis at some point.) In one study, half of the people with genital psoriasis said sex was painful and that they had it less frequently as a result. One third of people in the study revealed that their psoriasis in the genital area became more inflamed after intercourse. Given this, it’s important to talk with your partner.
Pregnancy
It’s super important to speak with an MD who specializes in psoriasis about family planning well before you conceive. Some psoriasis treatments—such as methotrexate, Soriatane (acitretin), oral retinoids and Tazorac (tazarotene)—can’t be used while you’re pregnant or nursing, and it may take time to get these medications out of your system. (For instance, acitretin can take several years to be cleared.)
Biologics are typically discontinued during pregnancy, too. However, many treatments like topicals, phototherapy, and some oral treatments can be used if you’re nursing since they don’t get into the breast milk, or the amount is negligible. Anecdotally, some people say their skin cleared somewhat or even completely during pregnancy, while others say it got worse. Some women say their psoriasis flared after giving birth; others say it didn’t. Reactions vary from person to person and can even vary in one person from one pregnancy to the next.
Because genetics play such a huge role in developing psoriasis, you may worry about having a child who has this condition, too. If you’re the only parent who has it, your child’s risk is 14%; if your partner has it, too, it’s 40%.
Where Can I Find Psoriasis Communities?
Top Psoriasis Instagrammers
Nitika Chopra, @nitikachopra
Follow because: You want to talk about taking your condition and turning it into something good—something that could quite possibly change the chronic world? That’s this chick. She is a beacon of light and joy while living with psoriasis, and she’s the founder of ChronicCon conference.
Alisha Bridges, @alishambridges
Follow because: Her spots are visible but that’s not really what you see when you look at this tall drink of water. Her style and flair for life speaks way louder than her psoriasis, and we are here for all of it.
Sabrina Skiles, @sabrinaskiles
Follow because: She’s rocking life through the trifecta of challenges: psoriasis, breast cancer, and toddlers. Not even a flare-up or chemo keeps this mom from a fashion find, a yoga sesh (which she highlights on her stories), or school drop-off.
Caridee English, @carideeenglish
Follow because: As a finalist on America’s Next Top Model, CariDee is proof that psoriasis can't hold you back from your dreams. Despite living that glamorous model life, she doesn’t sugarcoat the mental hardships of living with psoriasis.
Reena Ruparelia, @psoriasis_thoughts
Follow because: She zooms in on the real flare-ups of her psoriasis, from palms to elbows to ankles. All with emotional posts that are just as raw. A minute or two scrolling, and you feel like you’re insta-besties.
Top Psoriasis-Related Podcasts
Psound Bytes. Brought to you by the National Psoriasis Foundation, this podcast takes medical information, including insights on diagnosis, treatments, and lifestyle, and puts it into patient-speak so patients walk away feeling: oh, now I get it.
The Psoriasis Geek. Scientist and health blogger Gemma Boak talks everything from seasonal flares to the mental game, nutrition tips, and inspirational stories of others thriving with psoriasis.
The Point of Pain. It’s part psoriasis pain, part #chroniclife pain, and part emotional pain through divorce and growing up. Psoriasis advocate Nitika Chopra dives deep on all of it and doesn’t hold back with guests ranging from leadership coaches to sex educators.
Top Psoriasis Support Groups and Nonprofits
The National Psoriasis Foundation. This non-profit has dedicated itself to the 8 million Americans living with psoriasis and psoriatic arthritis for more than five decades. And when we say dedicated, we mean dedicated. It hosts a robust online community, offers one-on-one counseling, and puts its money where its mouth is—the foundation has invested $19 million dollars in clinical research to help find a cure for psoriatic disease.
Overcoming Psoriasis on Facebook (@PSOWHAT) . Consider this group of more than 19,000 psoriasis warriors your sounding board: there to support anyone looking for answers to life with psoriasis.
Experts aren’t sure exactly, but it’s clear that genetics and external triggers like stress, certain medications, and infections, among others, can cause the onset of and flare ups associated with psoriasis. Like many diseases, psoriasis is caused by a haywire immune system.
Both psoriasis and eczema are skin conditions that can be itchy and debilitating. But the similarities stop there. Psoriasis occurs typically as patches of thickened, scaly, inflamed, silver or red skin while eczema is dry and flaky in mild cases and red and irritated in those that are more severe. Eczema is also more common, leaving 10-15 % of adults and 20% of children scratching, compared to psoriasis, which affects around 3% of the population and usually hits later in life.
No. There is no test or tool to determine if you have psoriasis. Instead, your MD will determine that you have psoriasis and its type by looking at your skin with the naked eye and possibly via a microscopic biopsy.
Medicated shampoos are more effective for scalp psoriasis than traditional shampoo, but your doctor may prescribe other topicals including corticosteroids, scale softeners, a vitamin D3-based medicine called calcipotriene or tazarotene.
More Like This
What Black Dermatologists Want You to Know About Psoriasis
Medically Reviewed
From Eyelids to Toes: 10 Body Parts Affected by Psoriasis
Medically Reviewed
The New Psoriasis Guidelines That May Finally Get You the Treatment You Need
Medically Reviewed
Common Psoriasis Triggers—and How to Tame Them
Medically Reviewed


